Survive: Mountains (2016)
BASIC FIRST AID
Sometimes a survival situation arises because of an injury. It is imperative to know how to handle these situations calmly, correctly, and efficiently, while still only requiring minimal supplies and resources. This guide isn’t meant to be all-inclusive but should cover most emergency injuries.
BASICS
First step is scene safety. If you or the patient will be in danger of getting injured, or injured worse, you either shouldn’t approach the scene or should move the patient out of the dangerous area. Then try to keep as clean and sterile of a situation as possible, even if it is just washing your hand in a creek quickly before and after. Ultimately the most important thing is ABCC—in that order.
A—Airway
B—Breathing
C—Circulation
C—C-Spine
If somebody is seriously injured, the first step is activating your PLB or emergency beacon, if you have one, or sending someone for help. Then you want to make sure the patient’s airway is functioning, otherwise they won’t be able to get air in or out. Look in their mouth and thrust their jaw forward, without jostling the neck, to try to open the airway. Hopefully they will be able to exchange air and be breathing normally. If they are not breathing, start rescue breathing (mouth to mouth) and check their pulse every couple of minutes.
For C, you want to make sure there isn’t any major bleeding that would cause the patient to bleed out. If there is, take care of it through elevation, compression, and bandaging. If nothing is stopping the bleeding, start a tourniquet and make sure to write the time of application on the limb. C also includes circulation, as in making sure the heart is beating and perfusing the body. If the heart is not beating, chest compressions must begin and should be performed firmly and at a rate of 100 per minute along the breastbone just above the nipple line. Be prepared that if you are doing it correctly and firmly enough, you will probably break some ribs.
Finally, the last C stands for c-spine, which means cervical spine. These are the top seven vertebrae in the spinal column from the base of the brain through the neck to the bony protrusion at the base of the neck. These are the most susceptible to a life-threatening injury since if someone breaks the top two or three vertebrae they can immediately stop breathing. If there is a displaced fracture it can move and sever the spinal cord. If a c-spine injury is suspected, try not to move the patient and brace his or her head and neck with your hands, arms, or knees to try to prevent any movement at all.
EXTREMITY INJURIES
Extremity injuries are generally closed injuries and can usually be taken care of by splinting. If the patient is bleeding, make sure to stop the bleeding by applying a bandage and elevating the injury. A bandage can be as simple as wrapping strips of material, like someone’s shirt, around the injury. After controlling the bleeding, splint the injury to prevent movement. This requires splinting the joint above and below the injury if it is a long bone, or the bone above and below if it is a joint. Use materials that you have or can find to perform these functions. It can be sticks, pieces of driftwood, tape, trekking poles, and willows to secure the system.
If the fracture is open and bleeding, or if there is a loss of feeling, numbness, or tingling distal to the injury, you want to gently realign the injury into anatomical position before securing a splint to the injured area.
HEAD INJURIES
Head injuries can present in many different ways and can be very deceptive. It is important to monitor a person with a head injury accordingly. They may have minimal symptoms initially but can later present with a screaming headache, nausea, dizziness, vomiting, and some serious side effects that can come on hours after the event. These situations are very serious, and a rapid rescue from the backcountry is imperative.
Generally treat a head injury as you would most other injuries. Stop the bleeding, bandage to keep it clean, and compress the area, and monitor the situation to make sure things don’t deteriorate. Head injuries can be scary because they can include dizziness, repetition in speech, combative behavior, and almost drunk-like symptoms. Most symptoms will improve with time, but if things start to get worse, the situation has escalated and the injured party needs to get out of the backcountry as fast as possible.
+Tip: Willow bark has a similar active ingredient as aspirin. In fact, that’s where aspirin derived from. If you are not allergic to aspirin and have an injury, muscle pain, or fever in the backcountry, break off a piece of willow and chew the bark to release the salicin, or you can make a tea by steeping the bark in hot water.
COLD INJURIES
Depending on the season, temperatures in the mountains can get bitterly cold. Be prepared for cold injuries in this environment, especially if you are dealing with travel through snow continually. It is imperative to make sure that your extremities and core are warm.
Hypothermia
Snow will quickly melt into your clothing and zap your body heat without the proper layers. Be aware of the possibility of hypothermia. Dehydration and lack of food will also increase your chances of hypothermia.
To treat hypothermia, it is imperative to warm the body. The first step is typically to add layers or strip off the wet layers of clothing. Replace lost fluids and eat to maintain calories that will help warm the body.
Hypothermia can result in sluggish thinking, poor decision-making, loss of dexterity, and an unexplained feeling of warmth. Ultimately it will also lead to an inability to take care of one’s self, unconsciousness, and death.
It is crucial to rewarm a hypothermia patient as soon as you see the early stages. This can be done by body-to-body contact inside a sleeping bag or near a fire. Make sure to remove any wet clothing. In a serious case of hypothermia, take care not to rewarm the body too rapidly. Also once rewarmed, make sure not to let the body get cold again once removed from the heat source.
Frostbite
Frostbite is the result of frozen tissue. Frostnip is the first step as the skin gets cold and loses circulation. You may feel numbness or tingling before you lose feeling in the area. The longer it is exposed to the cold, the deeper the injured tissue will be and the more serious the injury. Be aware of the sensation in your face, feet, ears, and hands, as these are the most susceptible areas. Skin will look dull, whitish, and pale.
If you are with someone, they can monitor your face for the signs. If you are alone, you need to be aware of the loss of sensation to any of these areas. You can also periodically cover your nose and cheeks with a gloved hand to provide some warmth to the skin. If your hands are cold, place them in your armpits or groin to keep them warmer. Also make sure to scrunch and make faces and move your fingers and toes from time to time to increase the blood flow. If you lose feeling in your hands or feet, stop to assess the damage. If it doesn’t seem deep, rewarm the affected areas by using body heat or placing the injuries next to a hot water bottle. Do not insert the frostbite into hot or warm water. You want to rewarm the injured areas slowly.

+Tip: If you have or find ziplock bags, bread bags, or other plastic bags, these can be put over your socks or hands to create a vapor barrier liner and increase the warmth for your extremities by not permitting air exchange.

Most importantly, if you don’t believe you have the proper equipment to keep the area from refreezing, refrain from thawing the injured tissue. It will do more damage to thaw the area and have it refreeze and raise the chance of infection. Always avoid massaging areas with frostbite to rewarm them.
SNOW BLINDNESS
Bright sunlight in a snow-covered area can cause snow blindness. It happens when ultraviolet light damages the cornea. Initial symptoms include a feeling of grit in the eyes, pain in and around the eyes that often increases with movement of the eyeball, teary and red eyes, and a headache that usually increases with continued light exposure. Additional exposure can cause permanent eye damage.
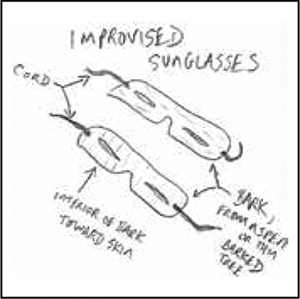
To prevent the condition, wear sunglasses or make a makeshift pair from tree bark, thin wood, or cardboard. You can also rub ash underneath your eyes to reduce the glare, as baseball players do with the eye black. To treat snow blindness, you will need to bandage your eyes and prevent exposure to light until the symptoms go away.
HEAT INJURIES
Mountainous regions are typically cool in temperature, but there is still the possibility of heat-related injuries.
Heat cramps are caused by the loss of salt from excessive sweating. Typically the cramps will be in the arms, legs, or abdomen. They will start as mild cramps but can gain in intensity. You should stop activity and take a break in the shade if the cramps begin. Make sure to drink plenty of water.
Heat exhaustion is caused by fluid loss and salt or electrolyte loss. Symptoms include headache, dizziness, mental confusion, irritability, excessive sweating, weakness, and pale, moist, clammy skin. If this occurs, immediately seek shade and water and rest out of the sun. Sprinkle the patient with water every few minutes and have them drink a small amount of water every 3 to 5 minutes.
Heat stroke is the more serious form caused by extreme lack of water and salts and the body’s subsequent inability to cool itself. This is a serious condition and could lead to death if the patient is not cooled immediately. Symptoms include nausea and vomiting, mental confusion, unconsciousness, headache, dizziness, and most importantly, a lack of sweat and hot, dry skin because the body isn’t functioning properly to cool itself. A person with heat stroke should be cooled by pouring water on them and fanning them.
ALTITUDE SICKNESS OR ACUTE MOUNTAIN SICKNESS (AMS)
In the mountains some people will feel the beginning stages of altitude sickness above 6,000 feet elevation. Above 9,000 feet, the symptoms can become more severe and require an immediate descent. The primary initial symptoms are headache, nausea, coughing, wheezing, difficulty breathing, and fatigue. Without descending to a lower elevation or giving your body a chance to acclimate, these symptoms can progress and become increasingly serious, and even lead to life-threatening health issues like cerebral or pulmonary edema. Make sure to drink plenty of fluids and listen to your body. If you are not feeling well, descend to a lower elevation. It is important to drink lots of water, since cold air contains less moisture than warm air and your body will be losing additional water to the outside environment.

DEHYDRATION
Everybody knows what dehydration is. The simple solution is to drink more water. It is important to mention that in cold weather you may not think you are losing fluids, but you still are. You may not need as much water as in warm climates, but you still need to check the color of your urine. Cold weather typically increases urine output, but decreases body fluids that you have to replace. If your urine is dark yellow, you are becoming dehydrated and need to drink more water.
SUNBURN
The sun can be intense at high elevations. Snow can also exacerbate the sun’s rays. Be aware that you can get sunburn even in below-freezing temperatures. The sun’s rays can reflect in all directions off the snow and can burn the bottom of your nose, the roof of your mouth if your mouth is open, or the back of your knees. If sunburn will be an issue, you can cover your skin with mud and let it cake in place to resist the sun’s rays.
