Ebola: How a People's Science Helped End an Epidemic - Paul Richards (2016)
Chapter 2. THE EPIDEMIC’S RISE AND DECLINE
The countries most affected by the 2013/15 Upper West African Ebola epidemic - Guinea, Liberia and Sierra Leone - occupy the bend in the Atlantic coastline, and straddle the transition from forest to savanna. They share much in terms of history and culture as frontier regions of the ancient Mali empire.
There are also significant differences. These stem in particular from the distinct modern political heritages of the three countries. Guinea was a French colony, and today uses French as its language of administration. Liberia was settled by the American Colonization Society as a home for free slaves, and became an independent nation from the mid-ninteenth century. Sierra Leone was a British colony and protectorate. The colony was founded at the end of the eighteenth century as a home for free blacks who had fought with the British army in the American Revolution. The protectorate was annexed at the end of the nineteenth century.
These similarities and differences are important in understanding the spread of Ebola and the international response.
Ebola began on the forest edge, in Guinea. This area of the Upper Guinean forest was settled at an early date by Kissi and Gola people, perhaps before or consequent upon the rise of the medieval Mali empire. The ethnonym ‘Gola’ is said to derive from the word for a nut with stimulant properties grown on the forest edge (kola), and traded widely throughout West Africa.
Paul Lovejoy states that this is ‘either an amazing coincidence or an indication that these people were identified through their participation in the [inter-regional] kola trade’.1 The neighbouring Kissi people were also brokers in trade between forest and savanna, especially in importing cattle from the savanna.
The long-established involvement of these forest-edge people in long-distance trade makes it apparent that the Ebola outbreak took place in an area in Upper West Africa quite different from the isolated hunting regions in the central African forests where earlier outbreaks had been experienced. Local populations on the Upper West African forest edge have over time developed extensive connections through trading partnerships and marriage that have spread over considerable distances.
Three braids of trade routes carried much of this forest-edge commerce both into the Niger basin to the north and down towards the coast. One braid (linking Sierra Leone and Guinea) followed the rivers north of Sierra Leone into the interior hills of Guinea, and towards the Upper Niger. The two others ran either side of the Gola forest as far as the segment of the forest-savanna transition zone from which the recent Ebola epidemic radiated. The initial spread of the virus was down the two routes skirting the east and west of the Gola forest, branching towards the coastal capitals Monrovia and Freetown.
Family, commercial and military alliances linked communities up and down these various forest-savanna routes, and help explain some of the networking among rural communities that accelerated the spread of the virus. Clan names, marriage alliances, the regional sodalities (Poro for men and Sande for women, sometimes called ‘secret societies’, because their activities, including burials, are known only to members), and shared institutional laws of hospitality connecting trading partners (landlord-stranger relationships) are commonly encountered. Disparate languages and lack of centralized state authority notwithstanding, the locality from which Ebola emerged is, historically, part of a culturally and economically integrated region only latterly divided up by colonially imposed international boundaries.
The three modern states began to take shape from the end of the eighteenth century. Portuguese established the first coastal trading links with the Sierra Leone peninsula in the sixteenth century. At the end of the eighteenth century British anti-slavery philanthropists founded a refuge for British army veterans of African origin in Sierra Leone. This became a Crown Colony (in 1807) and its port city - Freetown - a major base for British anti-slave trade patrols.
Anglo-French rivalry in the hinterlands of Freetown in the late nineteenth century led to the imposition of British and French colonial administration over the hinterland of these two port cities, and the emergence of French and English as national languages in two embryonic modern states, Guinea and Sierra Leone.
Meanwhile, Liberia emerged from the linking together of a number of coastal settlements for emancipated African-Americans, founded along somewhat similar lines to the British colony at Freetown. The British settlers were never free of colonial rule. In the Liberian case, however, the repatriated slaves formed their own independent government from 1847, though not without considerable tutelage, finance and military assistance from the United States of America.
The independent Liberian government exercised little control over districts in the interior beyond a forty-mile-wide coastal belt during the nineteenth century.2 At the end of that century both Britain and France began to entertain designs on the heavily forested Liberian interior. To protect its agreed boundaries the Liberian Frontier Force, with American military assistance, ‘pacified’ interior districts by force. This alienated many local communities, hitherto living independently, and triggered hostile attitudes towards Monrovia that linger to this day.
The international border between the three countries was finally settled by exchange of territory (a portion of the Gola forest) between Britain and Liberia in 1911. The old trade routes were then reshaped into today’s regional transport system, with major links homing in on Conakry, Freetown and Monrovia.
Ebola moved down these three distinct systems of communication much as raw materials (minerals and forest products) drained down them in the colonial period. This tree-like communications structure is most clearly recognized in Liberia, where people have a saying that ‘if we see you going we will see you come’. There are few if any lateral connections linking other centres in the country without the traveller passing through Monrovia.
Monrovia’s dominance over the lives of Liberians was reflected in the way Ebola so rapidly became an urban outbreak focused on the teeming capital.
For a time, Liberia outdid the other two countries in the rate of increase in Ebola infections. If this was due to the rapid arrival of the virus in a crowded, fast-moving urban setting, then we might see the early downturn in infection, beginning first in the heavily forested interior, as reflecting the power of indigenous institutions (notably Poro and Sande) in the Liberian interior. Some evidence (to be discussed in Chapter 6) suggests that local institutions were likewise effective in enhancing capacity to manage Ebola risks in Sierra Leone.
Guinea was different. The French ruled their colonial empire in Africa directly. They created a system that based its legitimacy on French legal codes and institutions. Institutions such as Poro and Sande were not recognized by the state as part of a system of ‘indirect rule’, as was practised in Liberia and Sierra Leone.3
At independence in 1958, the Guinean leader, Sékou Touré, refused President de Gaulle’s scheme of affiliation of former colonies with France. The Guinean president turned to the Soviet Union for help, and shifted the country towards a form of centralized, planned economy.
The Marxist regime waged war on obscurantism (traditional beliefs and institutions). This bore down especially hard on the people of the forest region who had resisted the spread of Islam, and retained beliefs associated with sodality membership, and respect for forest and ancestral spirits. In Sierra Leone the ruling political classes share an interior, forest background, but in Guinea the ways of thinking of the forest perhaps seem more remote to capital city elites, and long-Islamized mercantile communities.
Some of this suspicion between forest and coast was redoubled in Guinea by (the at times enforced) involvement of some forest communities in support for dissident military groups associated with competing factions in the civil wars in Liberia and Sierra Leone in the 1990s. Guinea also had its own forest-based rebel movement seeking to challenge the rule of President Lansana Conté. Conté had responded by sending helicopter gunships against the rebels.
This fraught history of relations between Conkary and the Guinean forest communities is reflected in episodes of hostility of villagers to Ebola responders, especially a widely reported incident on 16 September 2014 at Womeh, in Nzerekore prefecture, when a mixed delegation of medical personnel and government officials attempting to disinfect communities and explain Ebola risks were set upon by a hostile crowd. Eight of the responders were captured and killed.4
To summarize, there is a lot shared at the cultural level between communities across all three countries, but important differences are to be found in terms of national systems of governance (with Guinea remaining somewhat more closed and top-down in its systems of administration) and in patterns of integration between countryside and capital. In Guinea, Ebola was for a time enclaved within the forest region, remote in both terms of distance and mentality from the capital. In Liberia the virus very rapidly reached the capital, where downturn was assisted by a massive American military-led response. Downturn of Ebola in the interior of Liberia and Sierra Leone depended significantly on initiatives taken by strong local leaders (as will be discussed more fully in Chapter 6), especially those influential within the sodalities, where burial practices for important elders spread the disease.
Drivers of the epidemic
The Ebola epidemic in Upper West Africa began in December 2013 in the farming village of Meliandou, close to the city of Gueckedou (Gegedu), in south-eastern Guinea.5 It took some time to ascertain that this was an outbreak of Ebola, a disease hitherto unknown in Upper West Africa. Once the virus was identified responders assumed the disease would follow a similar path to previous outbreaks in isolated forest communities in the central African forests.
In these earlier outbreaks communities had been readily quarantined, in part through their own isolation, and infection contained. A major worry was recurrent spillover of the virus from intermediate hosts such as forest primates and human populations, especially hunters. Messages about Ebola hazards were strongly focused on the risk to forest-edge communities, especially from eating bushmeat.
Surprisingly for a disease thought to be a spillover from a forest animal host to humans (a zoonosis), the districts least affected by infection, once the epidemic began to spread, were those closest to the forest. In hindsight, this can be seen as a warning that this epidemic was different. Two of the seven chiefdoms containing the Sierra Leone portion of the Gola forest, Nomo and Tunkia, had no Ebola cases. In Liberia, Gparbolu County, an administrative district containing much of the Liberian portion of the Gola forest, was also free of cases (see Figure 2.2 below).
A problem with the international Ebola response still gathering momentum at this stage was that too much emphasis was placed on reducing the risks of zoonotic spillover. Populations in all three countries were repeatedly ‘messaged’ about the dangers of bushmeat, to the point where this was the single most widely known (supposed) fact about the epidemic.6 At times, people claimed they were immune to infection because, for reasons of religion or taste, they never ate bushmeat. Others were openly sceptical about the message, asking, ‘if the virus was so dangerous why didn’t all the animals die?’7
Emphasis on zoonotic risks in the early stages of the epidemic reflected a misreading of the environment where the first cases occurred. Meliandou is a farming village with a hunting tradition. Hunting is one of the markers of social identity in a country where forest communities have a history of troubled relations with savanna-based ruling elites. But the village is located on the margins of a small city (Gueckedou) where people are highly engaged in commerce, and cross the international borders with Sierra Leone and Liberia at will. Ebola in Upper West Africa first spread among farmers oriented towards trade and not towards forest subsistence.8
A historical vignette will help set the social scene in the epicentre of the disease. My colleague, the late Dr Malcolm Jusu, once told me that his grandfather, a Kissi warrior from Sandeyalu, in Kissi Kama chiefdom, in Sierra Leone, but adjacent to the Guinea and Liberia borders, maintained three homes, and depending on which government - French, British or Liberian - approached him for tax would relocate himself, his followers and his animals in one or other of the neighbouring countries to avoid payment.
This kind of long-established portable cross-border identity laid the basis for family networking intensified by armed conflict in all three countries in the 1990s. War either side of the new millennium visited the Sierra Leonean, Guinean and Liberian parts of the forest belt at different times. These disturbance were accompanied by much temporary shifting across borders, to seek refuge with in-laws, until peace and stability returned from c. 2005.9
As already noted, market-based mobility across borders is no new thing in the region where Ebola first took off. In 1893, on the eve of colonial conquest, Thomas Alldridge, a British travelling commissioner, introduced his account of what he termed an ‘ordinary native market’ in Kissi country, with the remark that ‘I think I shall be able to show that these [Kissi] people are not at all in the wretched condition often pictured by the European imagination’.10
He then lists the diversity of products available for sale, bought and sold in a local currency, Kissi pennies, made by local blacksmiths. This was the first point in his journey north at which Alldridge saw ordinary periodic markets. Further south, all the trade was in the grip of colonial traders based on the coast.
Intense, locally managed forest-edge trading activity not only survived colonial conquest, but was in fact further stimulated by the exigencies of the new international boundaries trisecting the region. In 1932 the British in Sierra Leone allowed a large international market to open at Koindu,11 at the northern tip of Kailahun District, practically on the Guinea border. This market became famous for, among other things, its international trade in African cloth. Some of this came from as far afield as western Nigeria, contributing the word hoku lapa (‘Yoruba [woven] cloth’) to the Mende lingua franca of the forest margins.12
Koindu market was closed because of the civil war in Sierra Leone (1991-2002),13 and kept inactive owing to subsequent armed disturbances in Guinea (1999-2000), and in Liberia (c. 2002-04), but was revived in 2008, after the region returned to peace. A contractor funded by the European Union began building a motor road from Kenema to the district headquarters (Kailahun) 2012.14 The road is supposed eventually to reach Koindu. To reach Koindu from Kailahun today requires a further 30 kilometres or so of travel over a single-track dirt road, alternately rocky and muddy. The at times nearly impassable state of this road contributed more than a little to the slow pace of the Ebola response.
Koindu is, then, no more than a mile or two from the two villages through which Ebola entered Sierra Leone, and these are a mere stone’s throw from the international borders with Guinea and Liberia.15 The market was once more closed in 2014, this time in response to Sierra Leone government restrictions on trade and movement.
The first officially recognized case of Ebola in Sierra Leone (25 May 2014) involved a nurse-midwife based in Koindu, who is said to have ‘treated a patient from Guinea, not knowing this patient had Ebola’.16 The closeness of Koindu to the Meliandou outbreak ought, perhaps, to have sparked an alert. Unfortunately the first message about Ebola to be circulated among chiefs in Kailahun District (in March 2014) was a warning about bushmeat,17 not about the dangers of human cross-border contact.
Spread of cases: a brief timeline
The WHO was first notified of an Ebola outbreak in Guinea on 25 March 2014, when numbers of cases were still small. The rate in Guinea levelled off from June to August, before rising more sharply in September, and finally reaching a plateau (with a much lower level of total cases than in Liberia or Sierra Leone) in December 2014 (Figure 2.1).
Cases in Liberia and Sierra Leone were first recorded in April and May 2014 respectively, and rose sharply from August 2014, sparking international concern and a major response. In Liberia numbers began to level off from October 2014. The same bend in the curve did not take place in Sierra Leone until January 2015. However, numbers were dropping sharply in eastern Sierra Leone from as early as October 2014. This is important to note because a downturn was evident before the main (British-supported) international Ebola ‘surge’ arrived.
Transmission ceased in Liberia from April 2015. Sierra Leone began a countdown to the end of the epidemic in late September 2015. Guinea began its final countdown in November 2015. Momentum in Guinea was assisted by successful ring-vaccination trials of an experimental Ebola vaccine reported to have good efficacy.18
Figure 2.1 Total reported suspected, probable and confirmed cases in Guinea, Liberia and Sierra Leone provided in WHO situation reports,19 25 March 2014 to 3 June 2015

Source: CDC
Gender and age: as factors in infection
Much of the infection risk from Ebola is borne by family carers. Babes-in-arms are at high risk when the mother becomes infected. Older children are at much lower risk. WHO data show that the age group 15-44 is three to four times more likely than children to be infected, and that the age group 45+ is four to five times more likely to be infected. Not coincidentally, these are the age groups most involved in nursing the sick and processing the corpse for burial.
The gender risks of Ebola have proved harder to pin down. Hewlett and Hewlett20 reported that females accounted for about 60 per cent of cases, based on data from earlier outbreaks. Data on adverse impacts of Ebola on survivors and survivor households for Sierra Leone21 also show a gender split in adverse impacts. This study sampled quarantined homes (including survivors and survivor households), and found that pre-existing gender biases against women were intensified among Ebola survivors.
Age bias was also intensified. For example, there was less water-carrying by women and more by girls in quarantined homes.
But WHO data, based on records for Ebola patients in hospitals and Ebola Treatment Units, show a 50:50 split between male and female Ebola victims. This seems consistent with evidence discussed in Chapter 5 on gender responsibilities, and thus distribution of infection risks by gender, in burial. Men prepare men’s bodies, and women prepare women’s bodies. There is an exception; in some Muslim households washing of corpses for burial - probably the most risky task associated with funerals - is reported as a special responsibility of women, irrespective of the gender of the deceased.
In sum, it seems clear the domestic burdens of women are intensified when the woman is a survivor, or living in a quarantined household. But it is not so clear that women are more at risk of catching Ebola than men, once age is taken into account. Men and women in middle age have responsibilities to the sick and dead that put both groups at risk of Ebola infection.
Picturing the epidemic as a breaking wave
In the earliest phase (December 2013 to July 2014) the Ebola epidemic was mainly confined to places on the flank of the Gola forest (Kailahun in Sierra Leone and Lofa County in Liberia). It was soon apparent, however, that the disease was mainly spreading along main roads and through market centres, and not along the forest margins.
Ebola rather rapidly gathered impetus to reach Monrovia, Conakry and Freetown, and Ebola responders faced for the first time the prospect of a large-scale urban epidemic. This caused major international alarm. Urban slums might prove massive multipliers for the disease. In the event, these concerns seem to have been somewhat misplaced. Responding was in some ways easier in urban environments since so much in Ebola prevention hinges on logistics (the rapid putting in place of effective communications, safe transportation and safe holding centres and treatment facilities).
All three cities possess sizeable port facilities and international airports, capable of handling the influx of materials, equipment and supplies needed for Ebola Treatment Centres. Urban cell phone coverage is good, and many city roads have been improved since the end of the Mano river conflicts of the 1990s. Urban community structures proved to be not noticeably less effective than their rural counterparts in supporting activities requiring citizen support, such as case-finding and quarantine.22
In all three countries, however, political responses were marred by delay. Fear of being blamed for the epidemic seems to have affected judgements. For example, the president of Sierra Leone did not visit Kailahun District, the disease epicentre in that country until 28 and 29 July 2014, six weeks after the outbreak was first reported, owing apparently to concerns that it was a heartland of the main political opposition.
Likewise, the government of Liberia appeared initially to have decided that the West Point slum in Monrovia was a no-go area, and ringed it with troops, who opened fire on protesters challenging quarantine. Later it became apparent that West Point had its own community structures, and that these were already effectively engaged in the fight against Ebola.23
Matters were perhaps most complicated in Guinea, on account of the long-term stand-off between central government and forest communities. Local suspicions of the political motives of central government in declaring an Ebola emergency clearly prolonged some infection chains in the Guinean forest zone.
Some differences in epidemic trajectory can be noted as a result of these variations in local political response. In Sierra Leone there was a prolonged period of rural spread with an eastern focus. Government agencies talked of trying to make Kenema a barrier to spread in the rest of the country, much as there was talk in 1991 of trying to stem a feared rebel advance by dividing the country along a line separating north and south.
But the barrier was all too readily breached by high-risk contacts, reacting against chaotic conditions for Ebola patients in the Kenema government hospital. Again, in recapitulation of the tactical circumstances in the civil war, fixed army checkpoints along the main road proved no deterrent to bike taxi riders prepared to explore bush path diversion, when paid well enough by quarantine ‘jumpers’.
In Liberia there was little the authorities could do to hold the epidemic wave at bay. The disease was a massive problem in the capital almost as soon as it had taken off in the interior.
Safe burial proved an immense challenge to the authorities in Liberia, who opted for a highly unpopular policy of compulsory cremations. Even so, ‘safe burial’ protocols were easier to implement when the bulk of cases were in one place. There were 2,000 Ebola cases in Liberia in August 2014. In the same period Sierra Leone had only 900 cases, but many of these were in rural areas inaccessible at the height of the rains. Kenema had, at the time, only one ambulance for ‘safe burial’, and it took up to four or five days to respond to some cases in villages. Faced with such delays, villagers took matters into their own hands, with unauthorized burials triggering further cases of infection.
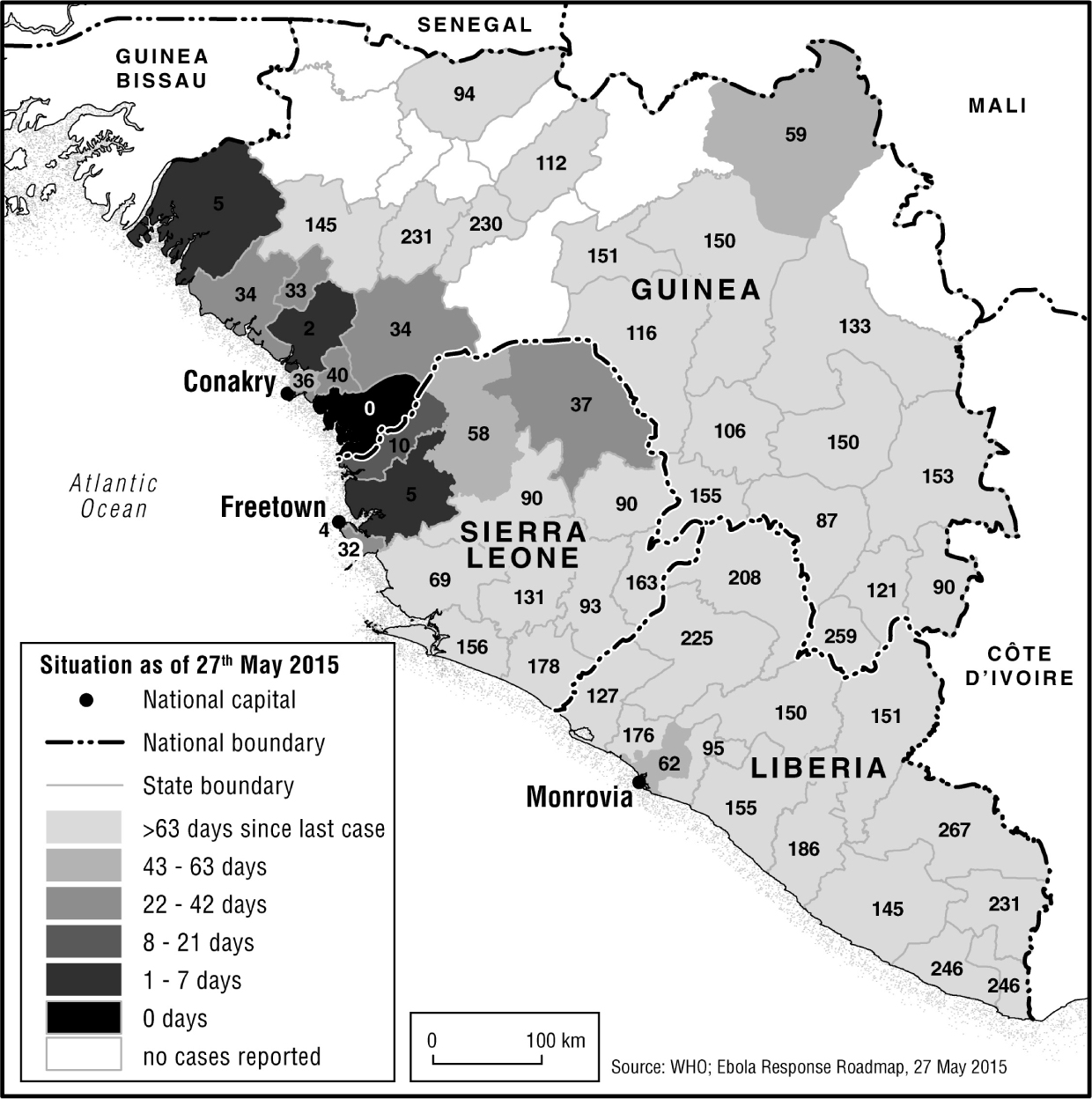
Even allowing for these nuances, however, the overall advance and decline of the epidemic is surprisingly similar across all three countries. The pattern can be likened to a wave - building, breaking and then ebbing. Infection ebbed first in places where the wave had gathered. Evidence of this is contained in three maps, Figures 2.2-2.4.
Figure 2.2 Where Ebola has been
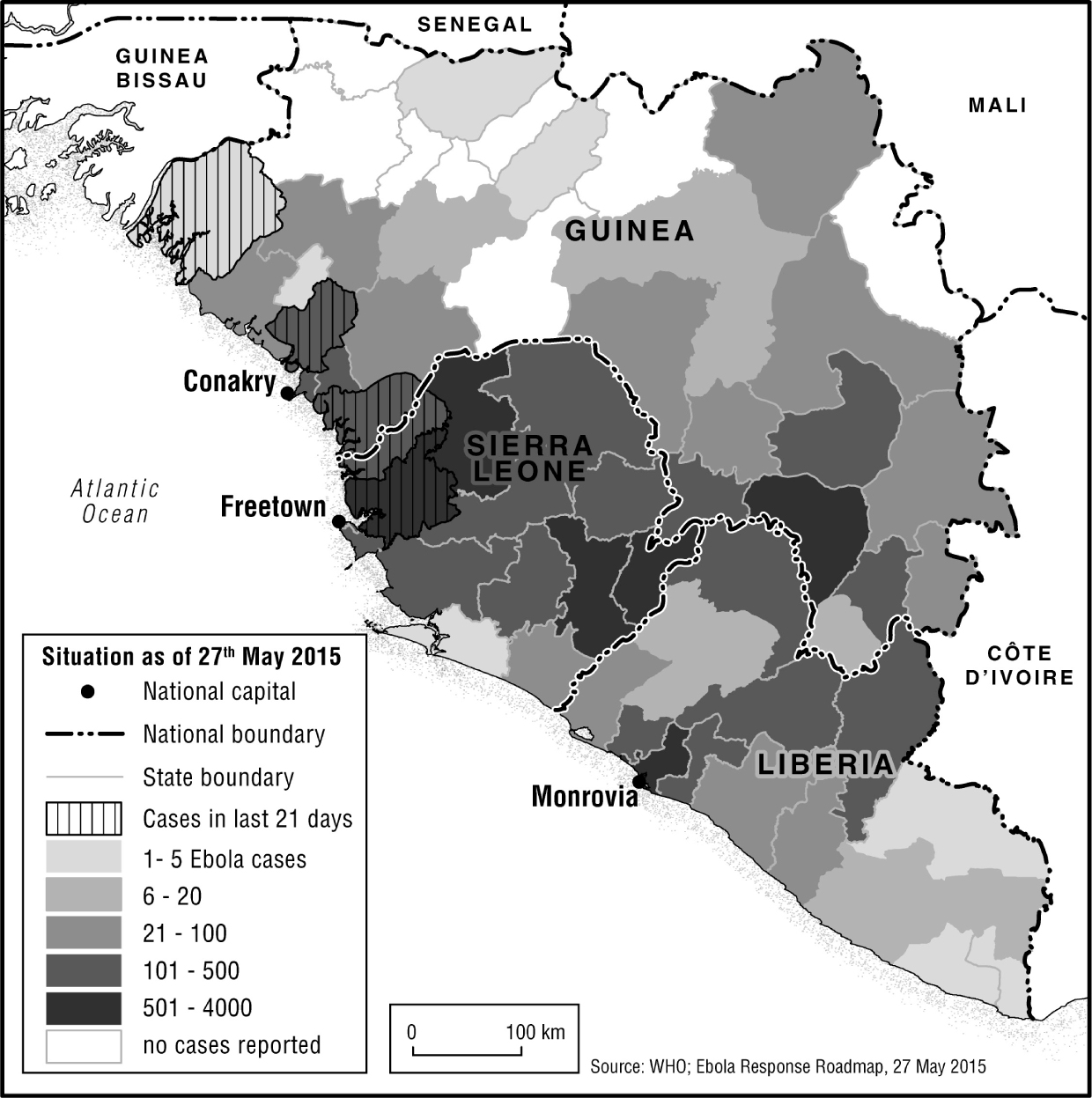
Figure 2.2 shows all localities where Ebola was or had been present up to May 2015; the disease reached almost all areas of all three countries apart from highland Guinea. Figure 2.3 shows the epidemic at its peak in late September 2014, with transmission still taking place in early-infected districts and also beginning to lap against some of the outer districts. Figure 2.4 evidences a general retreat of the disease in all early infected districts (including the whole of Liberia) by May 2015, with an active ‘edge’ of advance remaining across north-western Sierra Leone and coastal districts of Guinea, and reaching as far as the borders of Guinea-Bissau in the north-west.
Figure 2.3 Situation at 25 September 2014
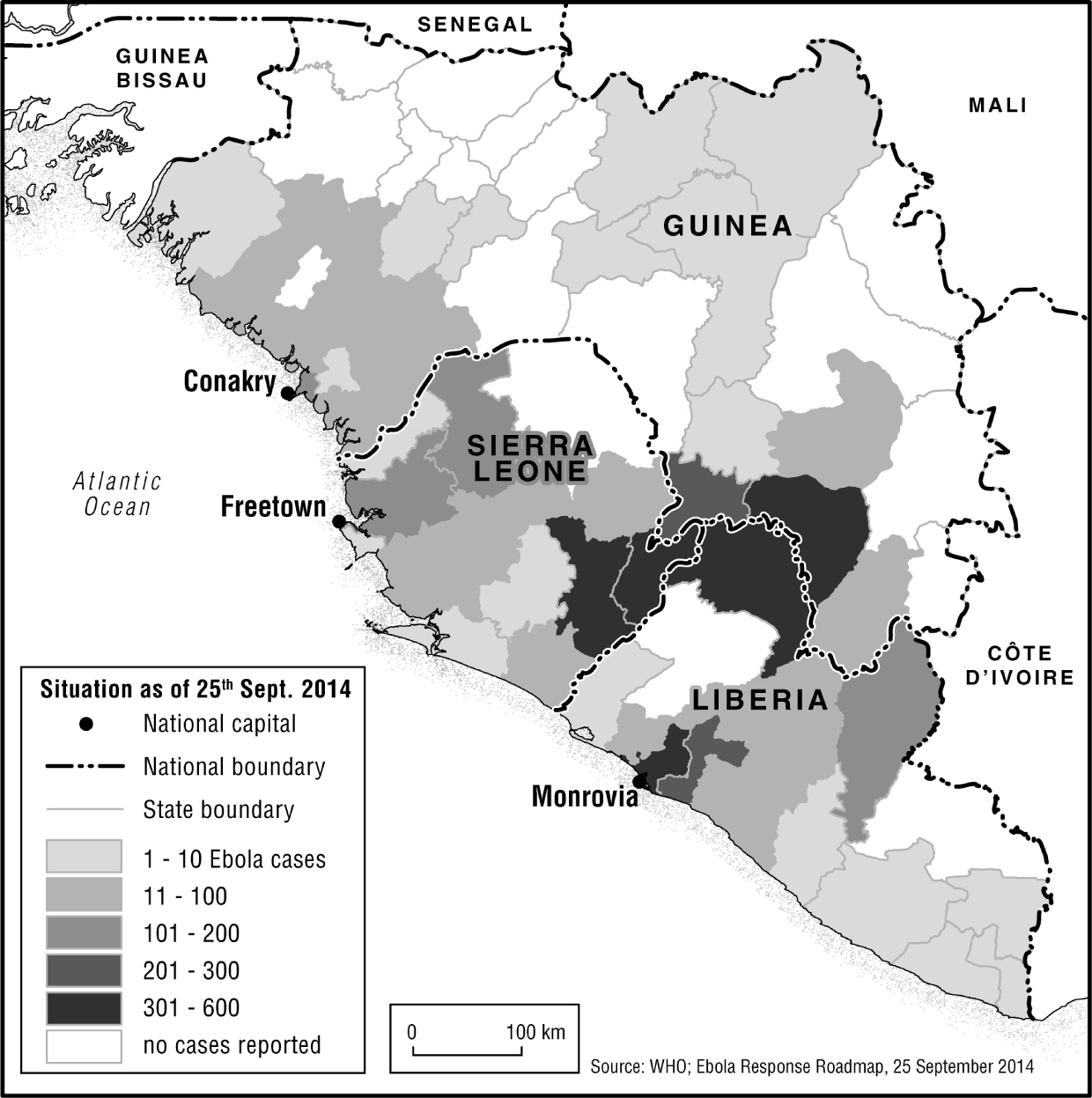
If localized variations in ecological, ethnic or political factors had driven the epidemic it seems unlikely they would have generated such a consistent wave-like pattern of early onset and early decline consistent across countries that are in many respects as different as they are similar. Seemingly the maps imply something common to the disease itself, such as burn-out due to a build-up of natural immunity, or a shared aspect of human response.
Acquired immunity among household carers has been reported, but the data have not yet been published.24 The linearity in the maps might also be explained in terms of logistics; clearly, responders built up their assets most rapidly in districts where the disease was most apparent. But there is also evidence (examined in Chapter 6 especially) that local response played a part in shaping the pattern of advance and retreat. Here the argument would be that communities figured out most rapidly how the disease worked, and what they needed to do about it, in places where caseloads were highest, and (in some cases) where access to external help was limited or delayed.
Figure 2.4 Situation at 27 May 2015
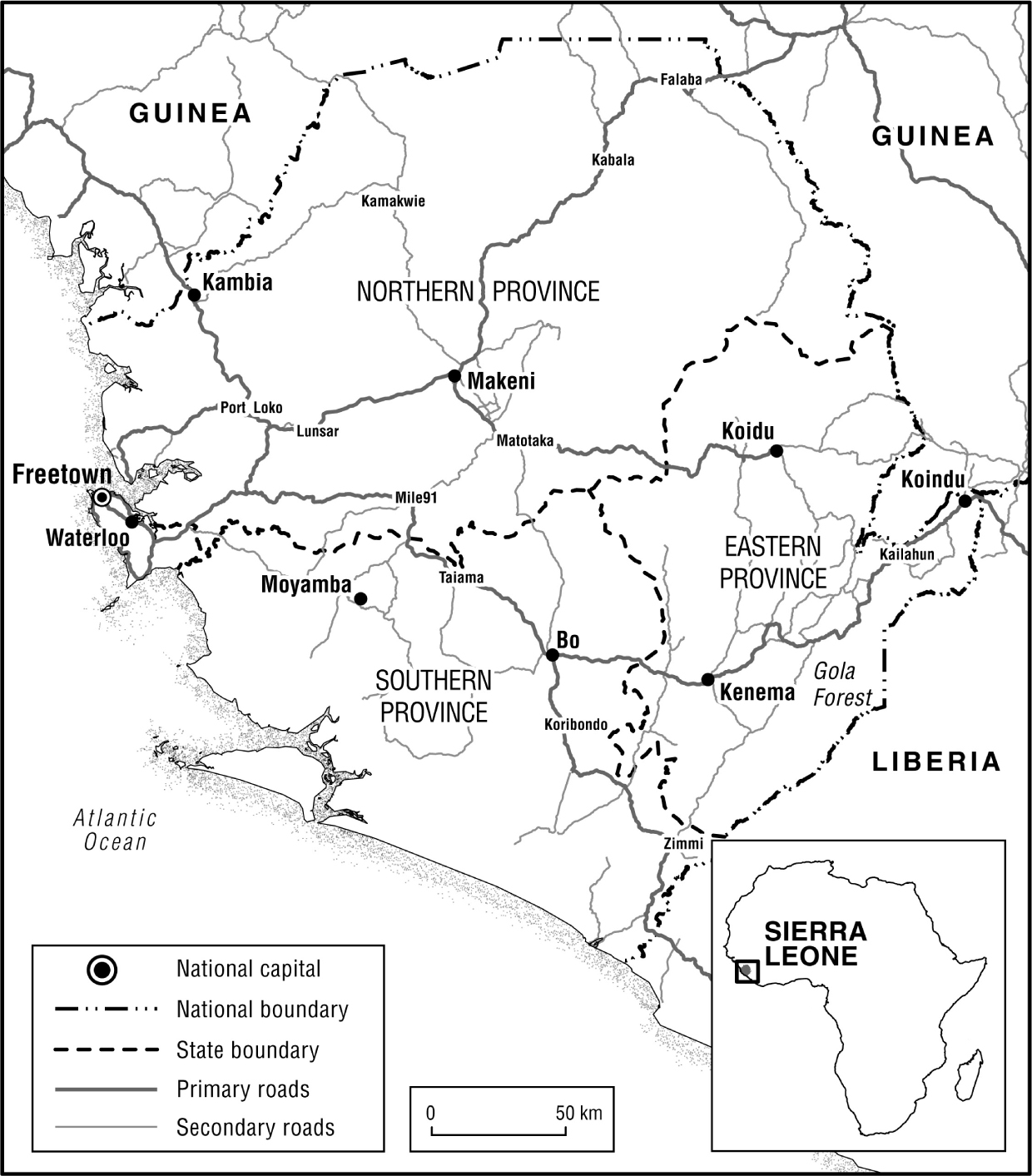
Of the residual factors, probably most attention should be paid to road transportation. The data for Sierra Leone are especially informative. Figure 2.5 maps the epidemic in Sierra Leone as it was in November 2014. Figure 2.6 shows the country’s main road system. The disease appears to have made a grand circular tour, starting in Kailahun, reaching Freetown and then spreading back up the main road system to the north of the country, finally completing the tour by arriving in the diamond districts bordering Kailahun on the west.
Figure 2.5 Extent of Sierra Leone epidemic in November 2014
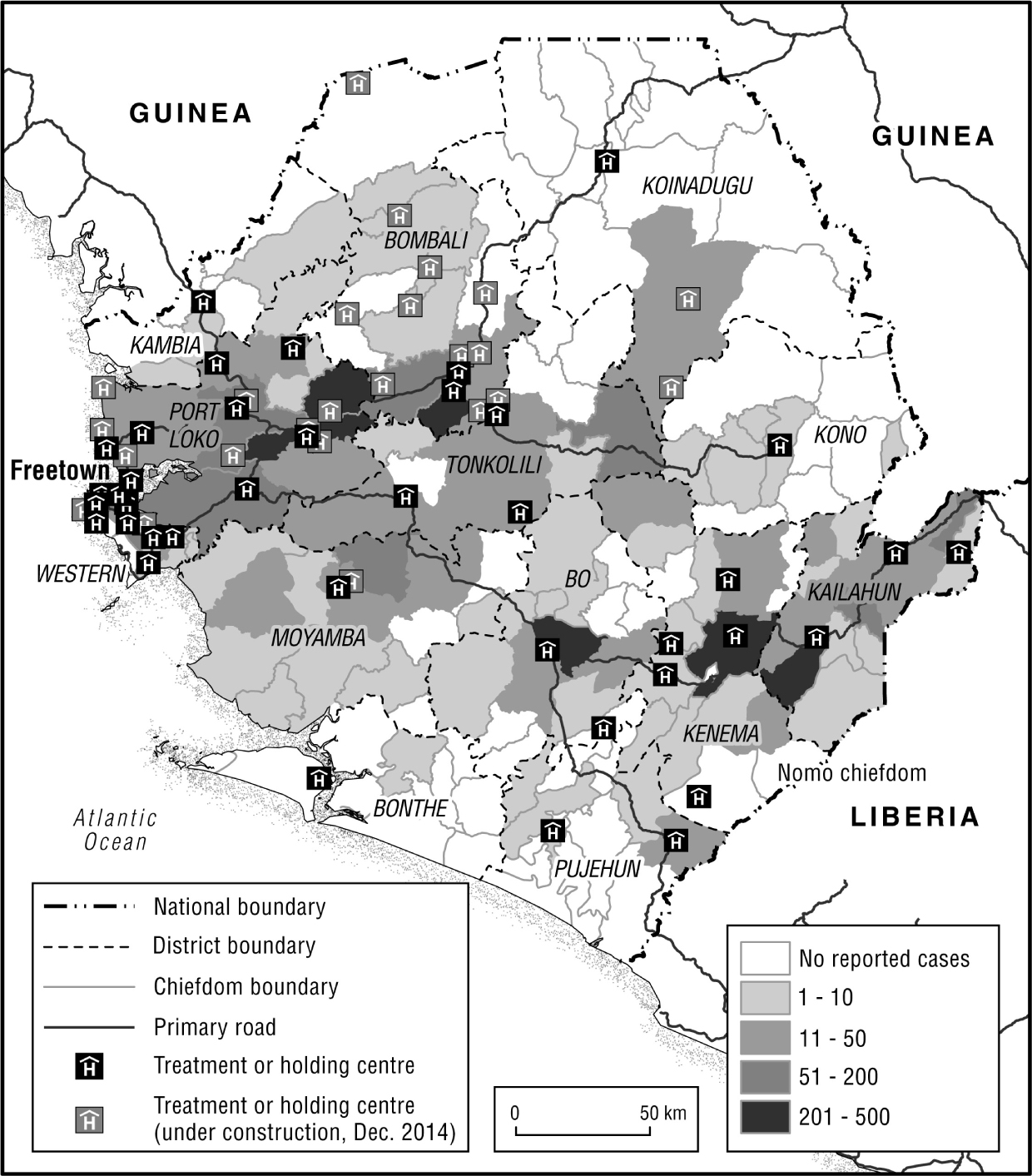
Clearly, properties of the transportation network were an important factor in the spread of Ebola at the national level in Sierra Leone. Areas on dead-end branches of the national road network seem to have been best able to keep the disease at bay. Pujehun, Bonthe and Koindaugu districts only ever recorded handfuls of cases.
Figure 2.6 National road system, Sierra Leone
Why social knowledge is important
Models are powerful tools in capturing the relevant features of an epidemic and provide projections to guide the planning of an epidemic response. But a model is only as good as the assumptions that go into it.
On 26 September 2014 the US Centers for Disease Control predicted that there might be up to 1.4 million Ebola cases in Liberia and Sierra Leone by 20 January 2015.25 The figure includes a correction for assumed under-reporting. There is also an important caveat that the number applies only if there are no additional interventions or changes in behaviour. Thus the prediction should perhaps be best understood as a warning rather than a projection.
The actual numbers of cases, in late January 2015, were as follows: Liberia, 8,524, and Sierra Leone, 10,491.26 In short, the model results were wildly wrong. But the caveat shows us what we should look for if we want to know why - namely, we need to consider the additional interventions and changes in behaviour that ended the epidemic. This is the theme for the remainder of this book. But to approach that theme it is helpful to explore in what respects the model was wrong. What becomes clear is that the model failed to incorporate relevant social information, including the extent to which carers acquired immunity.
Ebola is not airborne, but is spread only by contact with body fluids from a patient in the last phase of the disease. The risks of infection are largely confined to those nursing an Ebola sufferer, or involved in handling the body immediately after death. As noted above, such risks are mainly borne by older members of the family. Even neighbours are relatively safe, provided they keep a distance. In other words, risk of infection is not randomly distributed across the population, as the model assumes, but is strongly clustered. The risk is in fact largely confined to the immediate social group intimate with the Ebola patient. Models adjusted for social assumptions about the social clustering of infection risks yielded much lower predictions of epidemic growth.27
However, it is important also to point out that social intimacy does not always equate with residential proximity. Many families in Upper West Africa have rural origins, but live across a rural-urban divide. Ebola is, for this reason, capable of making unexpected jumps - unexpected, that is, to those unfamiliar with the geographical ramifications of the rural African extended family.
Research has documented these ramifications with regard to an apparently isolated outbreak in the remote village of Fogbo in Kori chiefdom, central Sierra Leone, in August 2014.28 Fogbo is situated on the Teye river, about eight kilometres by bush track from the main road running across central Sierra Leone from Freetown to Kenema. The first case in Fogbo was that of a man infected in Kenema, who had sought treatment from a member of his family in Fogbo, about 150 kilometres to the west. The man’s relative was a renowned herbalist.
There is no road to Fogbo, but the village can be accessed by motorcycle taxi along tracks leading to the far side of the river, crossed by canoe. Experiencing malaria-like symptoms, the sick man feared cross-infection with Ebola if he was hospitalized in Kenema. Evading checkpoints, he travelled to the village of his family member to receive local anti-malaria treatment. In Fogbo it is apparent that he succumbed to Ebola.
The man’s sickness triggered a local outbreak. The herbalist caring for him developed Ebola, and the family rallied to help her, but she died. Traders participating in the subsequent funeral of the herbalist took the disease back to the main road at Moyamba Junction, a main node for business in the area. A dispenser who had treated several of the Fogbo cases without realizing the risk then caught the disease, which was catapulted as far as Freetown when members of the dispenser’s Masonic lodge came to participate in his funeral. Ebola had reached from Kenema to Freetown in two bounds in a matter of days.
Long-distance movement in Upper West Africa was until recently restricted to motorable roads. But in recent years even off-road villages have been reached by motorcycle taxis. These bike taxis were a new phenomenon in Sierra Leone and Liberia after the civil war. Many of the bike riders were self-demobilized ex-combatants, unafraid to penetrate deep into the interior.29 There are today few villages in the three countries without some kind of motorized bike access.
The implication of the case material just discussed is that patterns of family interaction, and knowledge of how social knowledge is drawn upon to regulate these interactions, are highly relevant to any understanding of how Ebola moves. Modelling for Ebola needs to take account not only of clustering of risks due to family intimacy but also the jumps stemming from the enhanced mobility of members of the extended family group.
This poses an immediate problem for Ebola control. How can the disease be kept within localized pockets, without further pockets being cloned wherever high-risk contacts have intimate social connections.
One factor supporting Ebola control was already in place, throughout the three Ebola-affected countries. Rural people know those living around them very well, and this social knowledge serves to identify many of those who pose infection risks. A long-established institution of ‘landlord’ and ‘stranger’, widespread across the region, whereby any visitor comes under the protection of a member of the community, serves to keep family heads and chiefs apprised of movements of visitors into a settlement.
In all parts of rural Sierra Leone, for example, the presence of a stranger has to be reported to the chief, before that person is allowed to reside in a community, even for a night. This is to ensure the stranger is not maltreated, and that the stranger does not maltreat others. The requirement to report to the chief applies to persons arriving in a community to seek treatment for a medical condition.
A recent history of civil war across the region boosted this long-established rural system of social scrutiny. Villagers were alert to guard against infiltration by rebel spies and advance guards. Ebola has strengthened the legitimacy of this traditional monitoring system.
Urban and peri-urban communities also tend to reproduce the familiar village landlord-stranger system where they can. But landlord-stranger ties are less thoroughly applied in urban settings. In villages, strangers are readily noticed, and the eagle eye of the chief will soon be drawn to an unreported lodger. Visitors in an urban or peri-urban setting are much more numerous, and much more anonymous. Even so, neighbours are less anonymous than in large cities in Europe or America, and as a result Ebola contact tracing proved surprisingly effective even in urban areas.
Major exceptions are the mining camps and roadside trading centres, where people often come and go at will. Even so, chiefs will still often attempt to supervise visitors in these places because they have a financial incentive to do so. This is especially true in alluvial mining settlements in Sierra Leone or Liberia, where the chief belongs to a landowning family. The landowners participate in a share of the finds, and keep a close eye on those who might have diamonds or gold in their pocket. I knew one chief in Tongo Field, a long-established diamond area in Kenema District, who built his house with verandas at both back and front, in order better to scrutinize the adjacent workings without leaving his chair(s).
However, it is apparent from the Fogbo case that the landlord-stranger system is no guard against the spread of Ebola through family networking. As knowledge of Ebola risks intensified during the course of the epidemic, family movements often became subject to greater scrutiny, but the claims of family often overtook Ebola fears. Even in the countdown to the end of the epidemic some high-risk contacts were still evading contact tracing procedures, presumably accommodated by family members, perhaps unaware of their high-risk contact status. So any model for Ebola needs to spread the clustering of risks around family members, but also allow for some unexpected jumps consistent with the complex networking of Upper West African family life.
In short, to understand the dynamics of the Ebola epidemic in Upper West Africa it is necessary to understand the local social response. Analysis of this response is the task attempted in the remaining chapters.