Real Food: What to Eat and Why - Nina Planck (2016)
Chapter 9. Beyond Cholesterol
WHAT IS CHOLESTEROL?
When I told my friend Wendell Steavenson, an Anglo-American writer, I was writing a book about why butter is good for you, her comment was typically arch. “Cholesterol,” she said, mock solemn, “only exists in America.” I knew exactly what she meant. In much of the world—perhaps Wendy was thinking of London, Baghdad, Beirut, or Tbilisi, to name but a few cities where she has lived—people aren’t morbidly afraid of traditional foods like cream and lamb. Not yet, anyway.
The American anticholesterol campaign, which British experts gently mocked as “know-your-number” medicine, baffles foreigners. Here at home, it mostly inspires anxiety. When you sit down to eat with health-conscious Americans, the subject of cholesterol is hard to avoid, and the conversation seldom moves beyond weak jokes about clogged arteries.
We have been taught to fear this scoundrel called cholesterol, and fear it we do, yet most people have no idea what cholesterol is. It is often called a fat, but cholesterol is actually a sterol, a kind of alcohol. Cholesterol is part of all animal cell membranes. It makes up much of brain and nervous tissue, and it’s an important part of organs including the heart, liver, and kidney. It is so vital to the developing brain that defects in cholesterol metabolism cause mental retardation.1 Cholesterol is necessary to make vitamin D, bile acids (which digest fats), adrenal hormones, and the sex hormones estrogen and testosterone.
These roles are well known, at least to cholesterol experts. Then, in a college textbook, I came across a striking statement: cholesterol is a repair molecule. At first I didn’t understand it—or quite believe it. After all, cholesterol is known for doing damage, not healing. But apparently that’s not quite how cholesterol works. Let me explain by introducing the famous lipoproteins.
Low-density lipoprotein (LDL), often called the “bad” cholesterol, and its counterpart, high-density lipoprotein (HDL), or “good” cholesterol, are not forms of cholesterol at all, but vehicles. Like little boats with a waxy cargo, LDL and HDL ferry cholesterol around the body. LDL carries cholesterol from the liver to the tissues (including blood), and HDL carries cholesterol from the tissues back to the liver.2 In every healthy person, the lipoproteins help cholesterol go about its chores, digesting fats here and making estrogen there. The body needs both LDL and HDL. According to the Journal of American Physicians and Surgeons, the “good” and “bad” cholesterol story is “overly simplistic and not supported by the evidence.”3
Repair is one of cholesterol’s many tasks. When arterial walls are damaged, cholesterol rushes to the scene on a dinghy piloted by LDL to fix them.4 As the authors of Human Nutrition and Dietetics describe low-density lipoproteins, “their role is to deliver cholesterol to tissues for the vital functions of membrane synthesis and repair.” In Know Your Fats, Mary Enig writes: “Cholesterol is used by the body as a raw material for the healing process. This is the reason injured areas in the arteries (as in atherosclerosis) or the lungs (as in tuberculosis) have cholesterol along with several other components (such as calcium and collagen) in the ‘scar’ tissue [they’ve] formed to heal the ‘wound.’”
This could explain why high LDL is sometimes linked to heart disease. Many people with heart disease have damaged arteries, and cholesterol travels on LDL to heal them. Just because you see firefighters at burning buildings does not mean they start fires.
Cholesterol comes from two sources. The body makes cholesterol in the brain and the liver, which makes about 1,500 milligrams daily. The other source is the diet. Only animal foods contain cholesterol. It is stored in the fat of dairy foods and the muscle of animal protein. Thus beef, pork, and poultry, although they vary in fat content, have similar amounts of cholesterol (about 20 milligrams per ounce). That means trimming the fat from meat will reduce the fat but not cholesterol content, whereas skim milk contains less cholesterol than whole milk. Egg yolks and milk are particularly rich in cholesterol because baby animals need large amounts to build cell membranes and brain cells.
Experts once thought that eating cholesterol raised blood cholesterol. In 1968, they advised us to limit dietary cholesterol to 300 milligrams daily. This figure was not only unrealistic—with 275 to 300 milligrams of cholesterol, eating one egg would put you at or near the limit—but also arbitrary, as Gina Mallet discovered. Now we know that blood cholesterol is largely determined by metabolism—how the body makes, uses, and disposes of cholesterol. “The amount of cholesterol in food is not very strongly linked to cholesterol levels in the blood,” says a report from the Harvard School of Public Health.5
How much cholesterol do you need to eat? In theory, none; your body will make enough. But there are good reasons to consume cholesterol, which is harmless in its natural form. First, infants and children under two don’t produce enough; cholesterol must be part of their diets, which is why breast milk has plenty.6 The second reason to consume cholesterol applies to all ages: avoiding it entirely would mean shunning highly nutritious foods. Liver, meat, shrimp, butter, and eggs offer complete protein, omega-3 fats, and vitamins A, B12, and D—all vital nutrients not found in plants. It is not possible to separate the cholesterol from the nutrients in these foods. Older people may even benefit from eating cholesterol. In 1995, researchers found that cholesterol in eggs aids older people with declining memory.7
The body aims to keep cholesterol levels steady. Thus the more cholesterol you eat, the less the liver makes, and the less you eat, the more the liver makes. That explains why vegetarians and vegans, who eat few animal foods or none at all, can have high cholesterol. The 200-300 milligrams of cholesterol most people eat is less than half what the body produces. Moreover, up to 50 percent of cholesterol is determined by genes, not diet.8 As people with a family history of high blood cholesterol know, diet has little effect on blood levels.
If you have normal cholesterol metabolism, you may eat real foods without fear. As we’ve seen, people who eat traditional foods rich in cholesterol and saturated fat don’t have high cholesterol or more heart disease. Other traditional foods, meanwhile, have salutary effects on health in general and heart disease in particular; they include fish, red wine, chocolate, and olive oil.
Industrial foods are the real villain in heart disease. The main offenders are trans fats, corn oil, and sugar. As we’ve seen, trans fats promote atherosclerosis and clotting; polyunsaturated vegetable oils lower HDL; and sugar depletes B vitamins and raises triglycerides. All these effects are bad for the heart. The actual culprits are easy to spot for anyone who cares to read more than casually about diet and heart disease. So why did a perfectly useful molecule called cholesterol, which we’ve been consuming in liver, eggs, and shrimp for three million years, take the fall?
HOW CHOLESTEROL BECAME THE VILLAIN
The idea that diet contributes to heart disease is not new. In 1908, a young Russian medical researcher, M. A. Ignatovsky, fed rabbits a diet of animal protein, and when the bunnies developed arteriosclerosis, he blamed the protein. In 1913, a group of rival doctors followed by feeding cholesterol to rabbits, with similar results, including fat and cholesterol deposits in arteries, and they guessed that cholesterol, not protein, was responsible for the arteriosclerosis in Ignatovsky’s rabbits as well as theirs.
Animal experiments can, of course, be very useful, but in this case researchers may have reached the wrong conclusions. Unlike humans, who are born to eat cholesterol, rabbits are herbivores with no ability to metabolize it. When you force-feed rabbits with cholesterol, their blood cholesterol rises ten or twenty times higher than the highest values ever seen in humans; the effect is like poisoning. “Cholesterol is deposited in the arteries of the rabbit, but these deposits do not even remotely resemble those found in human atherosclerosis,” says Dr. Uffe Ravnskov, the author of The Cholesterol Myths.
Later, in human trials, researchers deliberately used oxidized cholesterol to demonstrate that dietary cholesterol causes atherosclerosis. Oxidized cholesterol, like oxidized or rancid polyunsaturated vegetable oil, is damaged and unhealthy. As I’ve mentioned elsewhere, it’s no secret in cholesterol circles that oxidized cholesterol, found in powdered eggs, powdered milk, and fried foods, causes arterial plaques.9 Dr. Kilmer McCully, author of The Heart Revolution, says that “pure cholesterol, containing no oxy-cholesterols, does not damage arteries in animals.”
Nevertheless, by the 1950s the cholesterol theory was well established: it was thought that eating cholesterol raises blood cholesterol and causes arteriosclerosis. Then, in a significant development, researchers concluded that cholesterol was not acting alone. The revised cholesterol theory had two parts: first, saturated fats (as opposed to unsaturated fats) raise cholesterol, and second, elevated cholesterol causes arteriosclerosis.
Ancel keys, the professor we met in an earlier chapter on fats, led the campaign against saturated fats. A prolific writer and speaker, Keys spent his last years in Naples, presumably enjoying the Mediterranean diet he had become famous for promoting. When he died in 2004, at the age of one hundred, his influence on diet and disease was rightly considered vast. Theodore Van Itallie wrote this tribute in Nutrition and Metabolism: “For those of us who worked … to call attention to the relationship of serum total cholesterol to risk of coronary heart disease (CHD), and to the cholesterol-raising effects of certain saturated fats, Keys will always be one of the major prophets who provided the early evidence that atherosclerosis is not an inevitable concomitant of aging, and that a diet high in saturated fat … can be a major risk factor for CHD.”10
In the 1950s, Keys made a series of contradictory statements about fats.11 He said that all fats raise cholesterol; yet elsewhere, he wrote that saturated fats raise cholesterol and polyunsaturated oils lower it. Keys said that animal fats caused heart disease; elsewhere, he wrote there was no difference between animal fats and vegetable oils in their effects. Clearly, his data were inconsistent. Nevertheless, Keys focused on one hypothesis: that a diet high in fat and saturated fat caused heart disease.
In 1953, Keys published a famous paper known as the Six Countries Study, placing fat and cholesterol at the center of the debate about diet and heart disease. Keys presented a diagram of fat consumption and death from heart disease in six countries; it appeared to show that the more fat people ate, the more deaths from heart disease. Japan was at the low end of the graph, which swept smoothly upward, and the United States was at the top. But the diagram didn’t tell the whole story. There were, in fact, data on fat and heart disease from twenty-two countries, but Keys omitted the other sixteen.12 Instead of forming a convincing upward curve, the twenty-two data points were scattered all over. He declined to cite Finland and Mexico, for example, where fat consumption was similar. Yet, inconveniently for the hypothesis Keys was promoting, Finland had seven times the rate of heart disease as Mexico.
In 1970, Keys published another famous paper—the Seven Countries Study—which appeared to demonstrate a link between cholesterol and heart disease in fifteen populations in seven countries. “The correlation is obvious,” said Keys. But when Ravnskov plotted Keys’s raw data into a graph, the correlation fell apart. The link is even weaker when you compare groups within countries. On the Greek island of Corfu, for example, people died five times more often from a heart attack than their fellow Greeks living on nearby Crete, although cholesterol on Corfu was lower.
Keys was undeterred and went on to advocate what he called the Mediterranean diet. “The heart of what we now consider the Mediterranean diet is mainly vegetarian,” he wrote. “Pasta in many forms, leaves sprinkled with olive oil, all kinds of vegetables in season, and often cheese, all finished off with fruit and frequently washed down with wine.” But the traditional Mediterranean diet is not chiefly vegetarian; beef, lamb, goat, pork, game, poultry, liver, and fish are common fare.
Pork—to name only one meat—is eaten throughout the region, where pigs (never fussy eaters) thrive on scrubby land. Italy and Spain are famous for cured pork (prosciutto and serrano ham) and for sausages, which require extra lard. The Spanish make sweet lard cakes called mantecados, while Italian bakers use strutto (rendered lard) much the way American and British cooks once did. In Tuscany, lardo di Colonnata—lard aged in marble with herbs—is eaten straight. In France, warm pork fat dressing and some kind of bacon are de rigueur in the classic salads pissenlit au lard and frisée aux lardons, made with the bitter greens dandelion and endive, respectively.
Olive oil is also traditional in the Mediterranean, of course. It’s eaten liberally on Crete, for example. (“My God, how much oil you use!” Keys is said to have exclaimed when he saw a green salad drowning in olive oil on the island.) But traditional Mediterranean cuisine includes many other fats, too. In northern Italy, butter is typical, and lard is eaten in central regions. In sprawling Provence, which spans the Mediterranean coast and the Alps, olive oil and lard are common, and Gascons are famous for duck and goose fat.
Although Keys was a central figure in the cholesterol hypothesis, he was not always invited to mingle with the nutrition establishment. Some people think this relative ostracism was due to his loner character and indifference to politics. I wonder whether Keys was excluded because proponents of the cholesterol hypothesis were threatened by his shift from blaming dietary cholesterol for heart disease to other factors, such as saturated fats.
The medical professor Stephen Phinney remembers a hallway encounter with Keys in the mid-1980s, shortly after the Lipid Research Clinic Coronary Prevention Trial demonstrated that the drug cholestyramine reduced cholesterol and coronary mortality. Keys showed Phinney a paper in which he examined HDL and mortality in Minnesota businessmen. In the paper, Keys wrote that HDL levels predicted heart-related deaths, but not death from all causes. Phinney recalled: “Dr. Keys was fuming, because this manuscript had been rejected by the major medical journals. Having set the cholesterol-lowering juggernaut in motion, the nutrition establishment was not about to let him sully the picture by demonstrating that it was not the only factor that determined important outcomes such as longevity. In his early 80s, Dr. Keys was still way out ahead of the consensus.”13
Later, Phinney told me why Keys, a nutritional epidemiologist, was unique in his field. “He understood the complexity of nutritional metabolism, whereas the pharmacologists either sought to reduce its complexity or ignored it. Pharmacology is a reductionist discipline—you always want to purify your drug and precisely define its target and its mechanism,” said Phinney. “This helps explain why diet and nutrition struggle for acceptance in the medical mainstream. The Mediterranean diet works better than atorvastatin”—the statin sold as Lipitor, which lowers LDL—“because it breaks the reductionist rule by harnessing the power of a combination of nutrients working against both cholesterol and inflammation.”14
Ancel Keys left a substantial legacy—and a complicated one. He was right to praise antioxidant-rich vegetables, monounsaturated olive oil, and fish. In 1994, the famous Lyon study found the greatest protection against heart disease in the Mediterranean diet was provided by omega-3 fats found in fish. He spoke of diet, rather than drugs.
Yet Keys also set the stage for a battle against the alleged dangers of saturated fats in traditional foods such as butter—dangers that were oversold, by Keys himself, by the medical-pharmaceutical complex, and by the U.S. government, which collectively took up the anticholesterol campaign with enthusiasm befitting a crusade.
THE CHOLESTEROL SKEPTICS
The old advice—butter ⇒ high cholesterol ⇒ heart attack—was too crude to be accurate. New advice is more subtle; experts advise us to avoid all trans fats, and we know that high HDL is good. The USDA is still far behind. In 2016, the section on oils in its educational materials on “Choose My Plate” still says, “Saturated fats, trans fats, and cholesterol tend to raise “bad” (LDL) cholesterol in the blood.” That’s only true of trans fats. Yet I have some sympathy for the researchers who reduced the message to an antibutter slogan. They meant well. If you labor in a complex field—and heart disease is certainly that—the appetite for simple answers can be maddening.
People will ask, If butter doesn’t cause heart disease, what does? Well, I venture, genes, lack of exercise, inflammation, free radicals, smoking, and industrial foods like trans fats, sugar, and corn oil. I believe this is accurate and reasonably complete; I hope it’s also brief enough to keep people from nodding off. I don’t envy doctors, who are forced by the clock and by anxious patients to reduce complex disease etiology, diagnosis, and treatment to three-minute summaries.
On diet and disease, this is as simple as I can make it without doing injustice to accuracy or uncertainty: diverse traditional foods eaten in moderation are good for you. There are various ways to go about proving this. You can feed people corn or coconut oil, and see that corn oil lowers HDL and coconut oil doesn’t. You can observe whether people who eat extreme diets (e.g., all meat) get heart disease. And so on. Such studies convinced me that you can eat whatever you want—except industrial foods. If that satisfies you, close this book and enjoy a dish of eggs in butter. Those who would like to know more about heart disease may wish to read on.
The quintessential disease of civilization, heart disease was rare before 1900, and rare it remains in preindustrial groups. In the United States, the first heart attack was reported in 1912, and by midcentury heart disease was the nation’s biggest killer. Today cardiovascular diseases—conditions of the heart and blood vessels, including angina, stroke, congestive heart failure, and heart disease—are still the leading cause of death. All cardiovascular diseases combined kill about a million Americans a year, men and women in pretty much equal numbers. Heart disease is responsible for 610,000 deaths every year. The South leads the nation in heart disease deaths.
There is also good news. Since peaking in the late 1960s, the death rate from cardiovascular diseases has fallen. In 1999, the mortality rate was less than 40 percent of the rate in 1950.15 Back then, heart disease was an acute, often fatal condition. After a heart attack, patients were simply sent home to rest and to die. Today doctors are adept at various treatments—drugs (blood thinners, beta-blockers, ACE inhibitors, calcium channel blockers), tiny balloons to open arteries, bypass surgery—so that heart disease, though still prevalent, is more often chronic than fatal. These advances keep many of the twenty-six million Americans with heart disease alive longer.
In the first stage of heart disease, angina, blood flow to the heart is restricted. When blood flow stops, it’s called a myocardial infarction, or heart attack. Together, angina and a heart attack are what doctors call coronary heart disease. Arteriosclerosis, or hardening of the arterial walls, is partly a function of age; with time, the smooth, elastic arterial cells become fibrous and stiff. Arteriosclerosis may be a protective measure to prevent the arteries from expanding under the pressure of blood; veins, which carry blood to the heart at much lower pressure, don’t stiffen in this way. When arterial walls become thick and swollen, it’s called an atheroma; many atheromas are known as atherosclerosis. Atheromas, which contain calcium, cholesterol, and fats, may burst, causing blood clots or heart attacks.
The long-reigning cholesterol hypothesis holds that saturated fats raise cholesterol and cholesterol clogs arteries, but a number of researchers, some of whom belong to a network called the International Committee of Cholesterol Skeptics, are doubtful. “The truth is that the cholesterol theory has never been proven,” says Dr. Kilmer McCully, whom I quoted earlier on oxidized cholesterol in powdered eggs. “Elevation of blood cholesterol is a symptom—not a cause—of heart disease.” Writes Ravnskov, a leading skeptic and the author of The Cholesterol Myths: “When the cholesterol campaign was introduced in Sweden in 1989, I was very surprised. Having followed the scientific literature about cholesterol and cardiovascular disease superficially for years, I could not recall any study showing that high cholesterol was dangerous to the heart, or that any type of dietary fat was more beneficial or harmful than another. I became curious and started to read more systematically. Anyone who reads the literature in this field with an open mind soon discovers that the emperor has no clothes.”16
At first I thought the skeptics might be few in number, but I found them all over. In 1978, a National Institutes of Health conference held to discuss the drop in death rates from heart attacks since the 1960s was unable to account for the decline by changes in fat and cholesterol consumption or blood cholesterol.17 Yet this statement got little attention. In 1998, a British National Health Service review found that blood cholesterol alone was a “relatively poor predictor of individual risk.”18 The authors concluded that for the general population, “cholesterol screening is unlikely to reduce mortality and can be misleading or even harmful.”
As you might imagine, the cholesterol skeptics have not received a hearty embrace from the medical and pharmaceutical establishment. In Finland, supporters of the anticholesterol campaign belittled Ravnskov’s book on television, and then—literally—set the book on fire. When I read The Cholesterol Myths, I got excited too, but it didn’t put me in the mood to burn books. Quite the opposite: it made me want to buy them. I began to read medical journals and textbooks, and soon I was a skeptic, too.
Does saturated fat raise cholesterol? Not in unhealthy ways. Early studies did show that certain saturated fats, when compared with polyunsaturated oils, raise total cholesterol, but now we know that total cholesterol is a poor predictor of heart disease. In fact, saturated fats raise HDL and polyunsaturated oils lower it. The National Cholesterol Education Program is clear about the virtues of HDL: “the higher, the better.” The general effect of saturated fats is to restore a healthy balance of HDL and LDL. Coconut oil, for example, raises HDL if it’s low, and lowers LDL if it’s high. As we’ve seen, certain saturated fats (stearic acid in beef and chocolate, and palmitic acid in butter and coconut oil) are good for HDL and LDL ratios.19 There is also evidence from traditional diets to absolve saturated fats. In Nigeria, for example, the Fulani get half their calories from fats, half of which are saturated. Despite what the theory predicts, they have low LDL.20
Does high cholesterol predict heart disease? In a striking number of cases, the link is weak. Since 1948, researchers have studied the residents of Framingham, Massachusetts, a city near Boston. After a few years, directors of the now famous Framingham Heart Study reported findings that became the bedrock of the cholesterol hypothesis: when they sorted people by low, normal, and high cholesterol, those with high levels had more fatal heart attacks. But almost half the heart attack patients had normal or low cholesterol. In Russia, a twelve-year study of more than sixty-four hundred men found those with low cholesterol had more heart disease.21 A study in rural China found that neither cholesterol nor LDL was linked to heart disease.22
I could cite many other examples—and the cholesterol skeptics do, at length—but the point, I hope, is clear: in Massachusetts, Russia, and China, something other than high cholesterol must be to blame for a large number of heart disease cases.
Cholesterol may be a concern for a relatively small group of people: younger men at high risk of heart disease, such as those who’ve already had one heart attack. In 1987, the Framingham data showed an association between high cholesterol and mortality for men under forty-seven. But for men older than forty-seven and for all women, there was no association between cholesterol and death rates from all causes, including heart disease.23 According to James Wright of the University of British Columbia, compared with high blood pressure, obesity, diabetes, and smoking, cholesterol is the weakest risk factor for women and heart disease.
The Center for Medical Consumers believes that the heart disease-awareness campaign exaggerates risks for women. In 2013, cancer and cardiovascular disease were tied for first place as the leading causes of death in U.S. women, but nearly 80 percent of heart-related deaths occur in women older than seventy-five. Associate Director Maryann Napoli commented, “Though the Framingham Study found a strong association between … cholesterol and heart disease only in young and middle-aged men, the entire population was … instructed to fear this particular risk factor.” It’s not clear that women need to reduce blood cholesterol to live longer. Dr. Barbara Robert is a prominent statin skeptic at the Women’s Cardiac Center at Miriam Hospital in Providence, Rhode Island. She says, “The risk of putting a healthy woman on a statin far outweighs the benefit.”
The vast set of data from the prestigious, long-running Framingham study will provide rich research material for years to come. For now, consider this fact. According to Dr. William Castelli, director of the Framingham study, “the more saturated fat one ate, the more cholesterol one ate … the lower the person’s serum cholesterol.”24 When Castelli made this astonishing admission in 1992, it didn’t make news.
DIET FIRST, THEN MEDICATION
Suppose you are a doctor, and the patient sitting before you is a fit woman in her midsixties. According to official guidelines, she has “high” cholesterol of 261 milligrams and “borderline high” LDL of 153 milligrams, but her HDL and triglycerides are great. Current advice from the National Cholesterol Education Program is to keep total cholesterol below 200 milligrams and LDL less than 100. Those cholesterol numbers are supposed to apply to everyone. No considerations are made for age, sex, or other risk factors on the NCEP guidelines.
Some doctors would write a prescription for a statin drug, which blocks the liver from making cholesterol. Statins are a multibillion-dollar business in the United States and the biggest-selling drug in the world. Under 2013 guidelines from the American Heart Association and American College of Cardiology, thirty-three million people without heart disease are candidates for statins, including large groups, such as anyone over twenty-one with an LDL of 190 mg or more, and anyone age forty to seventy-five with diabetes. These are very liberal guidelines.
But back to our female patient. In this not-quite-hypothetical case, the patient was my mother, and I was glad her doctor didn’t prescribe a statin. Mom didn’t need to worry about her total cholesterol or her LDL. First, total cholesterol is a poor predictor of heart disease in women and older people. Second, her ratio of total cholesterol to HDL puts her in the “below average” risk category. Third, in women and men over sixty-five, high LDL means longer life.25
Statins are highly effective at reducing LDL, and studies show they can reduce the risk of dying of a heart attack in high-risk people. But some researchers have doubts. Benefits of statins for total mortality—or death from all causes, the gold standard in epidemiology—are small or nonexistent. In 2004, Britain was the first country to approve over-the-counter sales of a statin. The Lancet objected, noting that five major trials found that death from all causes was similar with and without statins.26 “Statins have not been shown to provide an overall mortality benefit,” wrote the Lancet editors.
Statins work for a fairly small group. “The people who benefit are middle-aged men who are at high risk or have heart disease,” Dr. Beatrice Golomb said. “The benefits do not extend to the elderly or to women.” Golomb, who describes herself as “pro-statin,” is a medical professor at the University of California and the lead investigator in a large study on statin side effects.
As with any treatment, benefits must be weighed against costs. Side effects of statins include muscle weakness, nerve damage, kidney failure, liver damage, and memory loss. A rare but serious side effect is the potentially fatal muscle-wasting disorder rhabdomyolysis. In 2001 a statin linked to thirty-one rhabdomyolysis deaths was withdrawn. Statins deplete coenzyme Q10, an antioxidant found in fish, pork, heart, and liver. Used to prevent and treat heart disease in the United States and Japan, CoQ10 prevents LDL from being oxidized.27 “The first thing I do with new heart patients,” says cardiologist Dr. Peter Langsjoen, who has reviewed many studies on CoQ10, “is take them off statins.”28
What constitutes healthy cholesterol levels is also a matter of debate. The National Cholesterol Education Program says total cholesterol under 200 milligrams is “desirable.” But this target is not particularly useful. First, “total cholesterol” is not really cholesterol at all, but a composite number equal to HDL, LDL, and 20 percent of triglycerides. We now know that total cholesterol does not predict heart disease. Despite the bad press, high total LDL is a poor predictor, too. Recall that only half of heart attack cases show high LDL. Other readings such as triglyceride, blood sugar, and the inflammatory-marker C-Reactive Protein (CRP) may be more useful.
There are at least five major types of lipoproteins, including high-density, intermediate-density, and low-density forms, all of which enable fats and cholesterol to move within the water-based solution of the blood. There are at least four types of LDL, from large, “fluffy” LDL to three increasingly dense forms known as medium, small, and very small LDL. The very small or very low-density LDL particles called VLDL are now regarded as a chief culprit in atherosclerosis. VLDL is made in the liver from triglycerides, cholesterol, and apolipoproteins.
The dynamic actions of all the known lipoproteins have now been described in detail in expert papers. Any added detail is certainly valuable, but meanwhile, the related advice (concerning diet, lifestyle, and medicine) moves at a glacial pace. For example, eating natural saturated fats will raise levels of the large, benign LDL, without raising VLDL levels, but you won’t learn that from the National Cholesterol Education Program or the American Heart Association. Eating refined carbohydrates raises VLDL, while exercise and weight loss will reduce it, probably by reducing triglycerides.
All this we know about the LDL family. Yet it’s not yet part of routine conversations about cholesterol between patient and cardiologist. Why? Probably because there is no simple, direct way to measure VLDL; most labs use an indirect and imprecise calculation based on triglycerides.
Dr. Ronald M. Krauss, the director of the department of atherosclerosis research at Children’s Hospital Oakland Research Institute, would like to change that. He co-owns the patent on a machine that will separate LDL particles accurately by ion mobility analysis. He wants to be able to parse the common “lipid panel” most doctors order to produce more useful predictors of heart disease. Having studied the detailed lipoprotein profile of 4,800 Swedish volunteers, Krauss identified three scenarios that predict heart disease. The most powerful predictor has two parts: high levels of small and medium LDL and low HDL; the second, less powerful, scenario is low HDL; and the third pattern, which has the least predictive power in men, is high total LDL. Doctors can request ion mobility analysis from Quest Diagnostics.
Meanwhile, if, like me, you’re not inclined to submit to extra diagnostics, I recommend eating natural saturated fats, losing weight, and skipping refined carbohydrates. This will improve your (hidden) LDL subparticle profile—and, more important—reduce your heart disease risk.
Statins have fierce defenders and fierce critics. But when statins work—that is, when they not merely reduce a symptom (total LDL)—but actually prevent deaths from all causes, that’s reason to cheer. It now appears that the statin mechanism may be to reduce inflammation, a known risk factor for heart disease. If so, is there a better way to reduce inflammation and prevent needless deaths? Some doctors worry about reducing LDL at all costs. Attention has focused on “the supposed danger” of high blood cholesterol for fifty years, says Barry Groves, a British researcher on obesity, diabetes, and heart disease, while “the dangers of low blood cholesterol levels have largely been ignored.”29 Older people, for example, benefit from high cholesterol. Death rates in the elderly from all causes, including heart disease, are greater with low cholesterol.30 Thus the Lancet advises doctors to be “cautious” about reducing cholesterol in people over sixty-five.31 Low cholesterol is linked to respiratory disease, HIV, depression, and death by violence or suicide. Low cholesterol is also associated with another serious cardiovascular disease: stroke.32
Cholesterol protects against infection, a well-known risk factor for heart disease. Infection leads to inflammation, which appears in the arterial walls of heart disease patients with normal cholesterol. A good measure of inflammation is CRP, a risk factor for heart disease.33 Women with high CRP and healthy cholesterol have twice as many heart attacks.34 Inflammation is caused by excess omega-6 fats, smoking, and gum disease, another risk factor for heart disease. Exercise reduces both inflammation and CRP, which is produced in fat cells.
Heart disease has many causes. That means there are no simple answers in diagnosis, prevention, and treatment. On the positive side, there are potentially many cures. For example, if my mother wanted to lower her LDL without taking drugs, she could eat more fish. Omega-3 fats reduce LDL, raise HDL, lower triglycerides, prevent clots, reduce blood pressure, and fight inflammation. Fish is powerful stuff—and it has no side effects.
Another nutritional approach to reducing LDL is eating soy, almonds, oats, barley, okra, and eggplant. Dubbed the “portfolio” diet, this regimen compares favorably with statins in lowering LDL.35 University of Toronto researchers gave people with high cholesterol three treatments: one group ate a diet “very low” in saturated fat, the second ate the portfolio diet, and the third took statins. The statin treatment and the portfolio diet were equally good, each reducing total LDL by about 30 percent. The diet low in saturated fat was the least effective, reducing total LDL by only 8 percent. (The low-saturated fat diet, I noted, was also heavy on industrial foods: sunflower oil, fat-free cheese, egg substitutes, liquid egg whites, and “light” margarine.)
How does the portfolio diet work? Almonds are rich in monounsaturated fat, which lowers LDL. Soy isoflavones lower LDL. The viscous fiber in whole grains, okra, and eggplant also lowers LDL, perhaps by mopping up bile acid, which forces the liver to use up cholesterol to make more bile acid. The title of the editorial to accompany this small but promising study in the Journal of the American Medical Association was clear enough: “Diet First, Then Medication.”
A DISEASE OF DEFICIENCY
Kilmer McCully has indeed led a revolution because his work … has provided powerful evidence that nutritional deficiencies are an important cause of heart disease. Not surprisingly, this notion encountered great resistance … This is also the story of a personal struggle by a brilliant physician against a powerful and rigid scientific establishment.
—Dr. Walter Willett, Harvard School of Public Health
In 1968, Kilmer McCully was a young pathologist studying inherited diseases at Massachusetts General Hospital in Boston. One day, pediatricians told McCully about an eight-year-old boy who had died of a stroke at the same hospital in 1933. The case was unusual enough to be written up in the New England Journal of Medicine, and it made McCully curious. When he tracked down the original autopsy slides, he saw the severe arteriosclerosis diagnosed by the pathologist on the boy’s death thirty-five years before.
The boy had a rare genetic disease called homocystinuria, which is caused by faulty B vitamin metabolism and named for homocysteine, an amino acid that appears in the urine. Other symptoms include long limbs, mild mental retardation, and severe arteriosclerosis. Children with homocystinuria die of conditions one associates with old age: blood clots, heart attack, stroke. There is no cure, but high doses of vitamin B6 help relieve symptoms in about half of patients.
McCully happened to be familiar with homocysteine and cholesterol metabolism.36 In 1968, the leading theory of arteriosclerosis was that cholesterol attacked the arteries. But McCully didn’t believe cholesterol caused the damage he saw in this case. If cholesterol caused arteriosclerosis, why was there no cholesterol in this boy’s arteries? Mulling it over, McCully recalled animal studies linking deficiency of B vitamins and folic acid to arteriosclerosis, and he reflected on the cause of homocystinuria: faulty B vitamin metabolism. After many sleepless nights, his eureka moment came: McCully realized that excess homocysteine due to lack of B vitamins and folic acid caused arteriosclerosis. Cholesterol did not.
In 1969, McCully described his hypothesis about arteriosclerosis in the American Journal of Pathology and proposed a simple treatment: folic acid and B vitamins to keep homocysteine down. At first, this alternative theory of arteriosclerosis was big news, and scientists all over the world asked for copies of the article. In 1970, the hospital praised his work as an example of “the unpredictable, important contributions which can come when an imaginative, skilled worker is given free reign to follow his findings.”
But the warm reception was brief. The cholesterol hypothesis was still the establishment view; in 1968, experts had decreed that 300 milligrams of dietary cholesterol daily was the “safe” upper limit. As news spread of this apparent threat to the cholesterol theory, the medical world shunned McCully. He lost his research funding and his posts at Harvard and Massachusetts General Hospital. He went jobless for two years.
More than thirty-five years later, McCully was the chief of pathology at the Veterans Affairs Medical Center in Boston, and he regards the incident as a backhanded compliment. “If what I had discovered were unimportant, no one would have cared,” McCully told me brightly.37 He can afford to be magnanimous, because today the role of homocysteine is widely accepted. The landmark Physicians’ Health Study on diet and heart disease found that male doctors with high homocysteine were three times more likely to have a heart attack than those with normal levels. In the large and prestigious Nurses’ Health Study, women who ate the least folate and vitamin B6 had the highest heart-related death rates. The famous Framingham Heart Study also linked homocysteine to heart disease. McCully’s rehabilitation is complete. He is known as the “father of homocysteine.”
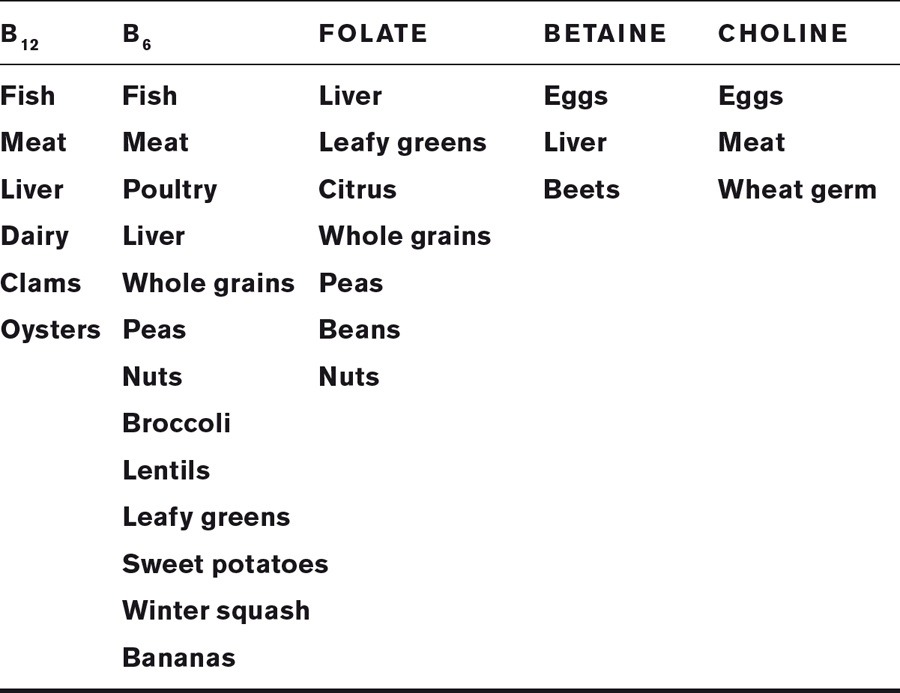
The normal role of homocysteine is to control growth and support tissue formation, but in excess, it damages the cells of arterial walls, destroys the elasticity of the arteries, and contributes to calcification of plaques. Vitamins help by reducing homocysteine. Folate and vitamin B12 convert it to harmless methionine, and vitamin B6 converts it to cysteine, which is excreted. Less well known nutrients betaine and choline also reduce homocysteine.
The actions of homocysteine fit with what we know about heart disease. It raises triglycerides and forms oxidized LDL, which causes arteriosclerosis.38 Homocysteine travels on LDL, which explains the high LDL seen in some people with heart disease. In addition to diet, many other factors—old age, menopause, smoking, diabetes, lack of exercise, being male, high blood pressure—raise homocysteine, and every one is linked to heart disease. “All along, it was homocysteine causing the damage,” writes McCully, “while cholesterol was getting the blame.”
A popular parlor game in cholesterol circles is solving the mystery known as the French Paradox. Why do the French have low rates of heart disease despite relatively high blood cholesterol and a diet rich in saturated fats? The French Paradox is only paradoxical if you believe that natural saturated fats cause heart disease, of course. But let’s pretend they do for the moment. Perhaps red wine is the answer, or smaller portions.
McCully believes the key to the mystery is the pâté, sautéed calves’ liver, and sweetbreads the French are so fond of. Liver and organ meats are superlative sources of folic acid and B vitamins, which keep homocysteine levels low. Homocysteine could also explain why people from Papua New Guinea to Nigeria eat liberal amounts of saturated fat and yet escape heart disease—another paradox for the conventional wisdom. Traditional diets are low in white flour and sugar (which deplete B vitamins) and rich in meat, liver, fish, whole grains, and green vegetables, all of which are good sources of folate and B vitamins.
WHAT TO EAT TO KEEP HOMOCYSTEINE LOW
Folic acid, vitamins B6 and B12, betaine, and choline reduce homocysteine. Note that B12 is found only in animal foods.
In the United States, voluntary fortification of foods with vitamin B6 and folic acid since 1950 may have contributed to the decline, since the 1955 peak, in deaths from vascular disease. Mandated fortification of foods with folic acid in 1998 may have further pushed the decline in mortality from vascular disease. Of course, real food is always preferable in my book.
To keep homocysteine levels healthy, eat beef, liver, oysters, eggs, whole grains, and green vegetables. Remember that vitamin B12 is found only in animal foods, especially salmon, tuna, cheese, eggs, liver, beef, and lamb. Also, nutrients are lost when food is processed. About 80 percent of folate disappears when whole wheat flour is milled into white flour, and vitamin B6 is easily damaged by heat. Thus canned tuna contains half as much B6 as fresh tuna. Vitamin B12 is more robust to heat, but microwaves damage nutrients much more than conventional heat.
McCully was not the first to blame industrial foods for heart disease, but his discovery about homocysteine was a giant leap forward in our understanding of how, exactly, refined foods damage the arteries.
“The first case of heart disease as it is known today was reported in 1912, the second in 1919, and since then it has developed into a major killer,” wrote Adelle Davis in Let’s Get Well. “The obvious change has been the ever-increasing consumption of refined foods and hydrogenated fats. The populations of the world living today on unrefined foods, in which nature packages with her fats all the nutrients needed to utilize them, do not develop heart disease.” She was writing in 1965. More than forty years later, Adelle Davis’s books are still worth reading. Even more remarkable, her work is cutting-edge.
BEYOND CHOLESTEROL
WHAT CAUSES HEART DISEASE
✵Deficiency of any of the following: omega-3 fats; folate, vitamins B6 and B12; antioxidants, including CoQ10 and vitamins C and E
✵Excess omega-6 fats (polyunsaturated vegetable oils)
✵Inflammation (from infection and excess corn oil)
✵Oxidized cholesterol (from free radicals in the body and powdered eggs and milk)
✵Sugar
✵Trans fats (hydrogenated oils)
A FEW RISK FACTORS
✵Age (84 percent of people who die of heart disease are sixty-five or older)
✵Excess weight, particularly belly fat
✵Sedentary lifestyle
✵Diabetes (also metabolic syndrome, or prediabetes)
✵Family history of heart disease
✵High blood pressure
✵High C-Reactive Protein (an indication of inflammation)
✵Kidney and gum disease
✵Menopause
✵Smoking
✵Thyroid disease
✵High blood sugar
✵High VLDL and low HDL