Manage Your Pain: Practical and Positive Ways of Adapting to Chronic Pain - Michael K. Nicholas, Allan Molloy, Lee Beeston, Lois Tonkin (2012)
Chapter 3. What’s Going On In Your Body When Pain Is Chronic?
Pain is experienced by people of all ages. However some people are born unable to feel pain. This may seem wonderful but these individuals may injure themselves without knowing it, as they don’t have pain to act as a warning system. Pain can be a very useful warning signal and can protect us from serious harm. But this really only applies to acute pain. Chronic pain doesn’t seem to have any useful purpose. By the time pain becomes chronic it is no longer acting as a warning signal. You’ve had it investigated so you either know what has caused it or you’ve been told you don’t have a serious injury or disease. But it can still be a mystery. Why isn’t it going away?
If you are confused about the basis of your pain or if you feel the doctors must have missed something, it can be difficult to accept ongoing pain. You may wonder if you do try to get on with your life, despite your pain, could you risk making things worse. This could leave you feeling unsure about what to do or where to go.
For these reasons it is important to learn a little about what can be going on in your body when pain persists even though you’ve had expert investigations and treatment. This will help you to understand the approach that is used in this book. This approach requires you to accept that you have ongoing pain but you are OK.
Summary
At any one time about 1 in 5 people experience some form of chronic pain, but the causes can differ between people. It often starts with an injury (like a broken bone) or an illness or disease (like Arthritis), but sometimes there is no clear reason. For example, with chronic low back pain a specific cause is often difficult to find. In many people the site of their pain may not be where the trouble lies, even though it feels like it. So, cutting off your arm may not fix the problem of chronic arm pain. In fact it could make matters worse.
As we mentioned in Chapter 1, recent research has shown that when we experience pain over a long time changes can develop in nerves in the spinal cord and the brain (the part called the central nervous system). These changes may not be seen on a scan but they can make us feel pain even when we seem to do nothing harmful. We call this a sensitization effect.
A common example of a sensitization effect is sunburn. When you have a shower with sunburned skin it seems to burn or sting. We know the effect is due to the sunburn not the hot water. When the sunburn settles the shower water stops stinging. This type of sensitization of your skin is called ‘peripheral sensitization’ and it is reversible with no lasting effects. Unfortunately, when the nerves in your spinal cord get sensitized it is not so reversible. This is called ‘central sensitization’ because it occurs in your central nervous system.
The key feature of central sensitization is feeling more pain when we do something that shouldn’t be painful, like a slight bump or just a handshake. Your doctor might call this ‘allodynia’. But if a mildly painful stimulus is felt as very painful your doctor might call that ‘hyperalgesia’. In both cases, the pain will seem quite out of proportion to the incident that triggers it. This can make you think there must be something seriously wrong and that you should avoid that activity in future. You might also worry that if you tell others about your experience they might think you’re imagining things or exaggerating. But, you’re not - these are common characteristics of chronic pain conditions.
There are two main types of pain. Nociceptive pain follows an injury to our skin, muscles, bones or tendons. This pain usually settles with healing, but not always. If it becomes chronic then it may come to involve changes in our nerves, like central sensitization. At this stage such pain is much harder to treat successfully.
Neuropathic pain is pain due to nerve damage. Central sensitization effects are a common feature of neuropathic pain and they are often long-lasting. These sensitization effects can also be experienced even when no nerve damage is found. In some cases this might be because nerve damage can be difficult to find, but in other cases it might be a more subtle effect of changes in our nervous system that we don’t yet fully understand.
Regardless of how chronic pain starts, all pain involves a chain of events in your nervous system, with one thing leading to another. The final stage of this chain of events is the pain you feel. Before that moment, pain is really just a lot of activity or signals in your nervous system. It is your brain’s job to make sense of this activity and interpret the signals as ‘pain’. Some of this ‘brain work’ will be outside your awareness, but some will be more conscious, especially if you can stop and reflect on it.
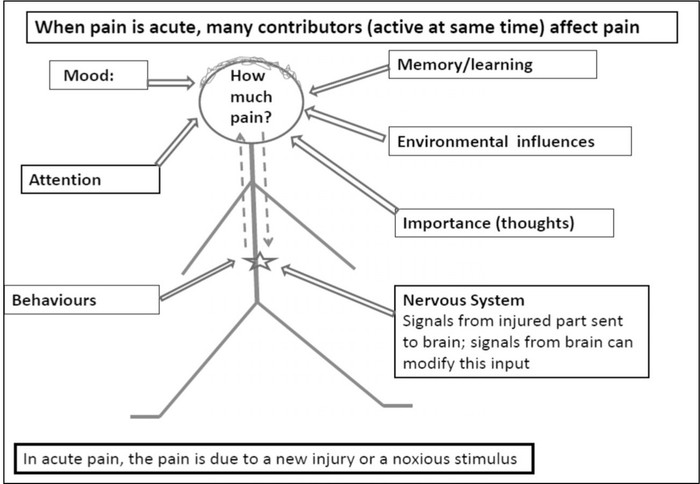
What your pain ends up feeling like depends not just on nerve signals coming up your spinal cord to your brain, but also on how you view the experience. If you see it as threatening you are likely to experience it as more severe and disturbing. But if you see it as something understandable and not threatening then it will seem less severe or disturbing. The diagrams in the boxes provide a simplified demonstration of what happens in your body when you have acute pain, using a lower back pain as an example, and what happens when the pain becomes chronic.
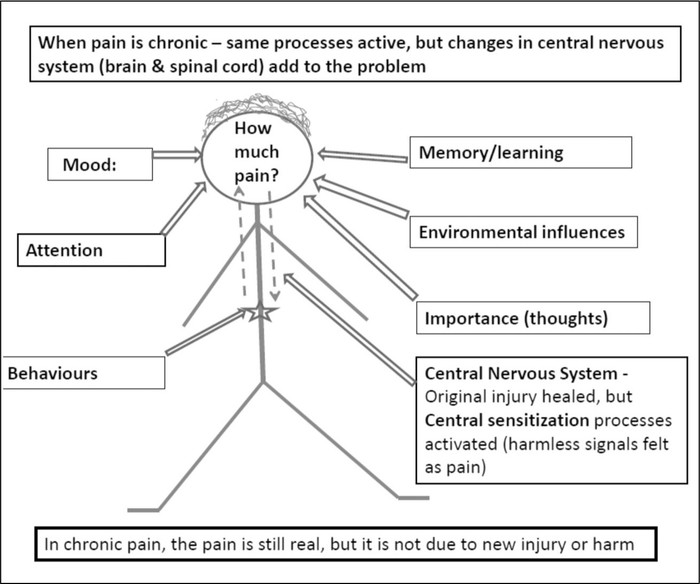
When the pain becomes chronic these contributors are repeated over months or years. It is easy to see how they can become learnt responses that occur almost automatically.
In the next sections we briefly describe the chain of events that can lead to the development to chronic pain like you have been experiencing.
Nervous system
1. From skin to spinal cord
Damage to our skin (like a cut or burn) or a sprain (like a sprained ankle) turns on small sensors close to the surface of the skin or tendons or muscles. These sensors are called nociceptors (related to the term “noxious”, meaning harmful). This is the first stage in the experience of pain. The nociceptors are linked to nerves end in the spinal cord (inside the spine). The messages (which are in the form of electrical signals) travel from the nociceptors, along the nerves to the spinal cord which sends them to the brain. It is only when the messages reach the brain that we feel pain, providing we are awake or conscious.
In many ways this is like what happens in a telephone system, where electrical messages travel along telephone wires until they are converted to sound in the handset.
This can happen very quickly. To give you an idea of how quickly, think of how quickly you can pull your hand away from a hot pan.
Soon after an injury the tissues around the injury site start to change. This is part of the healing process. We notice things like swelling, some redness in the skin, as well as pain and the area can also feeling hotter. These effects are due to tiny gaps in the small blood vessels widening to allow through part of the blood called plasma that is rich in protein and cells that can fight infection. Next, specialised cells begin to lay down a very strong material called collagen to form scar tissue. In many tissues the normal cells can multiply to replace damaged tissue. Nerves can regrow as well, but unfortunately the spinal cord cannot. Recovery of sensation depends on the nerves regrowing down the correct tunnel or sheath.
As healing proceeds, the messages that signal pain gradually settle and so does the experience of pain. Even after major surgery, most people do not require much pain relief medication after 3-4 days. Patients are encouraged to get moving as soon as possible as this helps to reduce complications and to promote recovery.
2. Spinal cord and brain stem
The spinal cord also plays a key role in the experience of pain. The spinal cord is a collection of specialised nerves and cells that lie within the spine. There are connections with the nerves that carry information to and from different parts of our body. The spinal cord is like a complicated telephone exchange, handling information coming in from nerves all through our body. The messages from these nerves are then sent up the spinal cord to the brain. At the base of the skull the spinal cord is connected to an area we call the brain stem which is the lower part of the brain. The brain stem plays a role as a filter, deciding which messages are passed on to the brain.
Not all pain messages reach the brain. They all reach the spinal cord but their entry to the brain can be blocked. In 1965 two scientists, a Canadian called Professor Ronald Melzack and an Englishman called Professor Patrick Wall suggested that there was a type of gate within the spinal cord which allowed messages to pass through to the brain only if it was open. But if the gate is closed the pain messages wouldn’t get through. This gate can be opened or closed by other nerve messages. It is important to understand that this theory mainly applied to acute pain, not chronic pain. Since 1965 our understanding of the nerve processes underlying acute and chronic pain has developed enormously, but the basic ideas outlined in 1965 remain relevant, especially for acute pain.
It has been known for time that the gate in the spinal cord can be closed by nerve signals indicating pressure or heat. So, rubbing a painful area when you are injured can ease the pain you feel. Putting a hot or cold pack on the painful area can also help. These measures don’t fix the injury but they can block the pain signals for a short period. TENS machines and acupuncture may work the same way (see Chapter 6).
The gate can also be closed by messages coming down from the brain. So, if you can distract your attention from the pain, or if you are not distressed about the pain, you won’t feel it as much. In an emergency situation, like a car accident, you can be injured but not realize it because your brain is too busy dealing with practical tasks like getting out of the car. You may only notice the pain when you are starting to relax and realize you are still alive. All these examples indicate the gate, or modulation system, is working to limit the pain you feel. This allows you time to deal with an emergency before you have to deal with any injuries. This mechanism has probably helped all animals, including humans, to survive as long as we have.
Examples of this gating system are often reported by people injured while playing heavy contact, physical sports but not noticing the pain until the game is over. Similarly, many soldiers who have been injured in battle have reported feeling little pain until later. Unfortunately, it doesn’t seem possible to keep the gating mechanisms closed forever. So this mechanism mainly applies to acute pain.
Just as the gate can be closed by messages from the brain, it can also be opened by the brain. If, for example, you focus your attention on the pain and worry about what it might mean, the gate can be opened allowing more nociceptive signals through and you will feel more pain. This can also happen without any conscious awareness on your part.
In our research, for example, we have found that even saying things like “this is terrible”, “I can’t cope with this”, or “I can’t go on” can lead to pain being more severe and troubling. If you’re not sure about this, try a short experiment. Hold a few blocks of ice in your hand (with fingers closed around them) for about 2 minutes while you say these sorts of statements to yourself and see what happens to the pain. Put the ice down, dry and rest your hand for a few minutes then repeat the exercise, but this time try saying things like “this is just ice”, “I know I’m OK”, and “I’ll just observe the sensation for a couple of minutes and see what happens”.
Compare the two situations - one where you are saying alarming things to yourself about the sensation, the other when you are more neutral and not alarmed, just curious. In both situations the noxious stimulus (the ice) is the same. The only difference is what you are saying to yourself about it. We call the alarmist thoughts ‘catastrophising’ and have found that when people think about their pain in a catastrophic way it hurts more and distresses them more. This means the experience of pain is not all due to the injury. It’s meaning to you also influences how it feels.
When pain becomes chronic the gating mechanism described by Melzack and Wall doesn’t apply as much because the original injury and source of the nociceptive signals has healed. Instead we have to look at other mechanisms in the central nervous system, especially the brain, to understand chronic pain.
3. The brain
The brain stem passes the pain messages up to an area of the brain known as the cerebral hemispheres or forebrain. This is the part of the brain that deals with thoughts, memories and emotions. It is only when this part of the brain has had a chance to make sense of the pain signals that we feel the pain that we know.
The brain tries to work out what the pain means to us. Which part of our body is it coming from? Should we worry about it or is it just a minor irritation to be ignored? Is it like something we’ve had before? What should we do about it? All these questions can happen in an instant and you may only be aware of them if you sit down and try to think them through later. The end result is that we can be acting on the pain signals even before we’ve really considered the best option to take. It can be as if we are on ‘automatic pilot’. In the case of acute pain that can be helpful. So the rapid response helps if your hand touches a hot pan and you need to withdraw it before it is badly burned. But if the pain is chronic and we are not in danger of being harmed the immediate response to an increase in pain may not be the best option.
In the case of chronic pain the pain signals are not a warning of new damage. Instead, they may be just normal sensations of pressure or strain that are misinterpreted by the brain as being a warning signal, like acute pain. This is the sensitization and amplification effect mentioned earlier. Remember the example of sunburned skin - the stinging pain we feel under the shower is not due to new damage. Instead the normal temperature shower water is felt as if it is much hotter than it is, because our sensitized skin amplifies the signals.
In the case of major damage to nerves, such as when a foot is amputated or the spinal cord is severed, no nerve signals can get through to the brain from below the site of the damage. But at least half of those people with these injuries report ongoing pain from below that point. We might call this ‘phantom pain’, but to the person with the pain it is not a phantom. In fact, this is an example of the brain responding to the signals it is receiving (and not receiving) from the spinal cord. This is an example of neuropathic pain, where there is clear nerve damage.
In these types of neuropathic pain there is often a mix of sensitization effects as well as the effects of the absence of expected nerve signals from below the injury site. It is as if the brain interprets not getting the normal signals from below the level of the injury as pain and other unpleasant sensations (such as itch and ‘ants crawling under the skin’). These other sensations can also be unpleasant even if not painful. They are examples of what is called “dysaesthesia”.
The longer we experience chronic pain the more these effects are repeated. It is not difficult to imagine a possible consequence of these repeated effects is that our responses to these repeated pain signals become learnt, like a habit. Like a habit they can be triggered by cues or reminders, often quite spontaneously. Just like a tune we haven’t heard for a while can stir dormant feelings in us. In the case of pain, a famous ballerina once reported that she just had to hear the music from one of her favorite dances to feel the pain she used to get from dancing on her toes. Similarly, some people with chronic pain report their pain can be stirred up even by seeing others obviously in pain. This is known as an empathy response.
If your brain is doing all this you might wonder why you can’t just block the pain out mentally and stop it. Unfortunately, no one seems able to do this very well or not for very long. But these observations about pain mechanisms do offer some clues for ways we might be able to combat chronic pain through our brain.
A key finding of recent research is that if your brain is receiving normal sensations from activities such as walking, exercising, swimming, and moving as normally as possible (that is, not too cautiously) then the pain responses in your brain can be reduced and the pain will trouble you less. This is especially true if you can accept the pain and stop fighting it or worrying about it (that is, not catastrophising). In general, leading as normal a life as possible and making the most of life can help to keep pain manageable and minimise its impact.
Another reason for resuming normal activities despite your pain is that it can help to disconfirm expectations and fears that something awful might happen. When you find you can do these things again and enjoy them, the pain will also trouble you less.
As you might have found with the ice experiment the significance of the pain (or what it means to you) can influence what you experience. If you can accept that the pain signals are not threatening and you are OK, you will experience them quite differently. They are just sensations, like background noise. On the other hand, if you repeatedly react to chronic pain as if it is acute (and a sign of new injury) you can remain in a state of distress which can make the pain feel even worse and more distressing.
You may not even be aware that these processes are playing such a major part in your experience of pain. Over time, these response patterns can become almost automatic, but you can become aware of the patterns and your responses. A cake once mixed and baked is very different to the individual ingredients from which it was made. Just as you can’t separate the ingredients of a cake so it may be difficult to separate the pain from your emotions, memories, thoughts, and beliefs. But understanding what is going on in your nervous system and realizing that chronic pain is not a threat to your body can help the process of accepting it and getting on with your life again.
4. Autonomic nervous system
This is a part of the nervous system over which we normally have little control but we can learn to influence it. It is made up of two parts: the sympathetic and the parasympathetic nervous systems. The sympathetic part controls our “flight and fight” reaction. If we are frightened and need to prepare ourselves for something that we think is dangerous the sympathetic nervous system causes changes like an increase in our heart rate and increased blood flow to the muscles. We also become more alert so that we can react quickly. The parasympathetic nervous system has the opposite effect - it slows us down.
Unfortunately, sympathetic hyperactivity (that is, over-activity) can occur even if there is no real threat. Being afraid of mice, harmless spiders or open spaces are common examples. The heart will race, sweating may occur and a feeling of anxiety is present. It may even lead to a panic attack. Pain can also produce this response which can be very distressing. Fortunately if the pain cannot be relieved, we can learn to control this response which should reduce any distress.
The sympathetic nervous system can also become hyperactive in a condition called reflex sympathetic dystrophy or complex regional pain syndrome. This usually follows nerve injury, but the nerve injury can be very minor in some cases. For example a hand or foot will become painful, stiff, sweaty and change in colour and appearance. As with other pain conditions there are a number of medical treatments that may help. But they are often not enough to resolve it completely and the approaches in this book should be included in the treatment plan.
5. Bones and the spine
Humans have an internal skeleton consisting of a backbone or vertebral column which is connected by specialised joints to the head, the arms and the legs. These bones and joints grow with the person. They provide remarkable flexibility and the capacity for a range of complex movements through the attachment of muscles, tendons and ligaments across the joints. Being upright, humans experience significant pressures on the bony skeleton. Movement adds to these stresses through the contraction of muscles anchored to the skeleton.
The anatomy of the spine
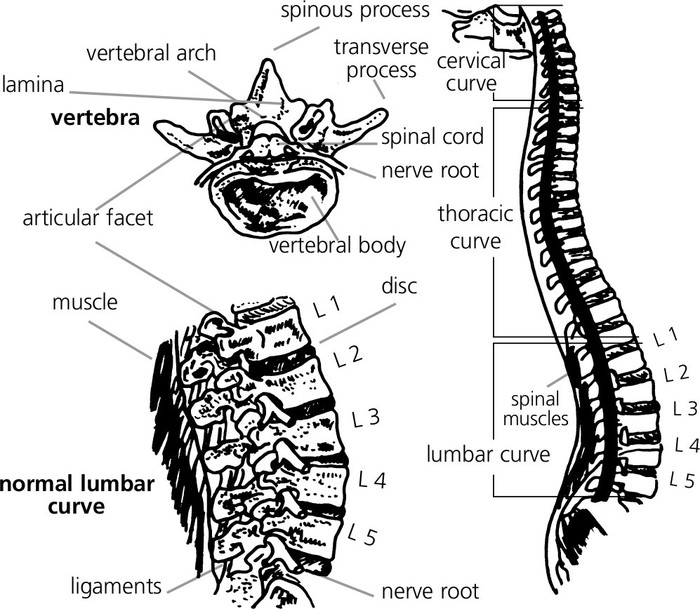
Within the protection of the backbone lies the spinal cord. This is linked to the brain through the base of the skull and to the body by nerves which pass through spaces between the bones which make up the spine. Messages travel to and from the brain to trigger sensation and activate muscles respectively as described above.
In this disposable consumer age we don’t expect things to last very long yet we expect the human body to last a lifetime, possibly at least 70-80 years. What makes it all possible is the human body’s ability to repair and regenerate itself. This is usually a slow process unless trauma occurs and then the body rapidly repairs itself.
As we get older the supple discs between the vertebrae (the bones of the back) become more rigid and fibrous, lose height and lead to restrictions in the amount of cushioning and movement.
Also with age the effects of wear and tear or spondylosis become apparent with thickening of the surface of the vertebrae and new irregular bone laid down around the edge of the discs. The lower lumbar vertebrae are affected most. This adds to the limitation of movement caused by changes in the discs and arthritis of the paired facet joints (see glossary) may also contribute. These changes start from about 30 years of age and progress at different rates depending on the individual. At the age of 60 years, wear and tear is evident on most x-rays. Calling these changes “abnormal” is wrong as they are clearly “normal” for that age group.
Surprisingly there is no clear relationship between the changes seen and pain experienced. An individual may have advanced degeneration of the spine yet experience little or no pain yet a younger person with a normal looking x-ray may have severe pain. A mistake is easily made here. Saying that backache is due to spondylosis may result in other important causes being missed. It is important that you don’t try to deal with “wear and tear” effects by avoiding activities. In general, keeping fit and active keeps us supple and healthy.
Vertebral slips. The bones of the vertebral column are held in position like the mast of a ship with muscles and ligaments acting like ropes. The articulations of the facet joints also provide stability. But as a result of wear and tear of the joints or if a break occurs in the bony arch at the back of the vertebra, it can slip forward, which is called a spondylolisthesis. This is present in 1.5% of the Australian population but is usually painless. A slip in the other direction is called a retrolisthesis. As this slip in the vertebrae can stretch the nerve roots pain in the legs may occur.
Narrowing of the vertebral canal: The canal inside the backbone in which the spinal cord lies varies in size in different individuals. In about 15% of the population the canal is tight, a condition known as spinal stenosis. It may have just developed that way or there may have been degeneration of the facet joints and discs that lead to ingrowths into the bony canal. The usual symptoms are numbness and pain in the back and legs on walking. This is eased by sitting and usually by bending forward as this seems to allow more space in the bony canal.
Joints: Each bone in the body is connected to at least one other. At this junction there is a joint of some type. There are many types of joint, for example the hip is a ball and socket joint whilst the ankle and knee are like hinge joints. The inner surface of the joint is lined by very slippery material to minimise resistance to movement.
Wear and tear can occur in these joints. This is known as osteoarthritis. Heavily-used joints, such as hips, knees, and the joints in the spine, develop roughened surfaces and in an attempt to repair this the body lays down new tissue. Around the edges of the joint bone is laid down. This can effectively splint the joint, restricting its movement. At the same time, within the joint an inflamatory process occurs. This makes the joint tender and can be painful. Over time, this pain may spread to surrounding areas. This is called referred pain. So, wear and tear of a hip may be experienced as pain in the knee.
Muscle: There are different types of muscle in the body. There is skeletal muscle which is the “red” muscle and smooth muscle which occurs in the lungs and bowel. The heart also has a special type of muscle. Skeletal muscle usually spans a joint. By contracting, movement of a joint will occur. Most muscles have an opponent, a muscle that will counteract the effect by having an opposite action across a joint. Unfortunately muscles will weaken if not used and lose their bulk. They can also shorten and in doing so limit the movement of a joint. When you try to use muscles in this state they tend to be painful for a period. Anyone who does unaccustomed exercise will be familiar with this phenomenon. Fortunately, with ongoing use, the muscles can recover and this pain lessens.
In certain conditions, however, there may be taught bands within the muscle, which may respond to stretching, but not totally. As a result some pain may persist. This is known as myofascial pain if it is localised to one area. If it is widespread it may be classified as fibromyalgia by some doctors.
Ligaments: Ligaments play an important role in support and therefore the movement of joints. There are two types of ligament. Most ligaments in the body are made from white fibrous tissue which is usually non-elastic and unstretchable. It will stretch but only after prolonged strain. There is another type of ligament that is elastic and will return to it usual length after stretching. This type is present between the bones of the back allowing the spine to bend. Stretch exercises can assist this process.
In summary, many structures in the body can contribute to chronic pain, either as a cause or a reaction to the effects of pain, especially disuse. None of these structural changes can fully account for what people with chronic pain actually experience. Many of the bodily changes with chronic pain are not structural but functional. That is, processes like central nervous system sensitization change the ways our nervous system functions. In this case, making the nervous system more sensitive. These functional changes can explain how normally harmless activities or stimuli can be experienced as pain. These functional changes cannot be seen on scans, but scans can rule out major structural damage. Some of these changes are modifiable, but not always completely. The options for treatment for chronic pain conditions will be addressed in the following chapters.