Ebola: How a People's Science Helped End an Epidemic - Paul Richards (2016)
Chapter 5. BURIAL TECHNIQUE
International responders at times talked about infection chains sustained by ‘stubborn’ villagers persisting in ‘hiding’ corpses and engaging in ‘secret’ burials. Thus it was important to find out more about normal burial practices, and why people felt aggrieved at not being able to follow their expected procedures. Fieldwork was carried out in December 2014 involving parallel focus groups for male and female elders and young men and women, in the hope of encouraging all age groups to talk as freely as possible about Ebola, and especially issues relating to burial technique, since this was an important point of friction and misunderstanding between Ebola responders and affected communities.
The ethnographic detail on burial technique is extensive. It is perhaps sufficient here to consider just two villages, Fogbo and Foindu. These are chosen because they are located on the main ethno-linguistic divide in the country, and had some direct experience of the disease. The Temne- and Mende-speaking communities in Sierra Leone are each estimated, in total, to comprise about 40 per cent of the national population, and by repute have different burial customs.
Care needs to be taken to avoid ethnic essentialization. The idea that fixed ethnic or linguistic affiliation drives burial practices is a further example of the doubtful notion that culture is causal. To draw on an example given by Mauss, the French and English troops in the Great War of 1914-18 used different shovels, and dug differently, because they had developed different practices on different kinds of land, not because they belonged to different nationalities.
The Yoni Temne of Foindu and the Kpa Mende of Fogbo share a common environment of grassland interspersed with patches of bush and riverine forest. There is considerable intermarriage across the border separating them, though more often Temne men marry Mende women, giving them access to more abundant land on the Mende side of the provincial divide. Many people along the border speak both languages fluently. Thus we perhaps ought to expect a continuum of beliefs and practices, not a sharp break.
In fact, the continuum is not entirely smooth. In former times, the boundary was militarily contested between the Temne polity of Yoni and the Kpa Mende state, with a major military concentration at Teyama (Taiama). A large river (the Teye) separates, rather than joins, the two groups. Although Foindu and Fogbo are only a few kilometres apart on the right and left banks of the Teye there is no significant river traffic between the two places.
Transportation and administration take the people of the two villages in different directions. Fogbo people take their major medical cases to Moyamba or Bo (Southern Province), while Foindu people seek medical assistance in Magburaka or Makeni (Northern Province).
Fogbo: a Kpa Mende village
Appendix 1 (see page 153) shows transcripts of segments of parallel focus group sessions held for male and female elders, and a mixed gender group of young people in Fogbo, a village in Kori chiefdom hit by an Ebola outbreak in July/August 2014. These were the first cases in Moyamba District.
In all three groups informants were prompted to talk about the process of handling the body from death to interment. These responses refer to ‘normal’ burial processes (i.e. what would have obtained prior to the requirement for compulsory ‘safe burial’).
The youth group provided a short, generic account, but covering the activities in which they would be involved, namely transfer of the corpse to the grave, and some details of the layout of the grave itself, which they would have helped to prepare.
The women elders spoke more times, but concretely, apparently about the burial of a specific person, without elaborating much on their largely factual answers.
The male elders group, by contrast, not only described specific techniques of body management in some detail, but also provided important interpretive insights on symbolic aspects, such as the fact that when the corpse is being washed in the backyard of the dead person’s house the head needs to be positioned towards the sun (the presumed direction of travel of the soul) or the soul will be disoriented, and remain on earth, tormenting family members.
The details about the inverted bucket placed where the feet rested when the body was washed are also informative, since it is stated that the soil under the bucket will be used to rub on the body of the wife or husband, to separate the living from the dead, so that the dead will have no power to inflict pain or bad luck on remaining family members. This seems a potential infection pathway for Ebola. In some cases a trench is dug under the washing platform to drain away the water, since this is thought to carry risk of infection.
In Bawuya, a small settlement close to Fogbo, the focus group for young people added that if it is the first time the wife/husband lost a partner, the remaining [partner] is washed ceremonially with part of the grave soil [and] water to avert bad luck/misfortune from the remaining partner.1
Both male and female elders in Fogbo describe the grave cloth given to the last child to wash in the stream and then keep. The men add moving detail about the river washing out and carrying away the soil from the grave, indicating the end of life, as the soil is carried away by the river. Presumably this cloth is a potential Ebola infection hazard, and should, under current rules, be burnt. WHO protocols for safe and dignified burial2 recognize that families will want to offer prayers at the grave, from a distance. But this is a static provision. There is no scope for an excursion to the river, and its poignant associations are lost as a result of Ebola restrictions.
Foindu: a Temne village
As a Temne-speaking farming village of about the same-size (population c. 500) a few kilometres upstream on the Teye river on the opposite (right) bank, and administratively located in Yoni chiefdom, Tonkolili District, Northern Province, Foindu is a good comparative foil for Fogbo. Foindu did not experience Ebola directly, whereas Fogbo did.
Male elders described what they knew of the Ebola ‘safe burial’ process: According to information, it involves placing the corpse in a plastic bag, spraying of the house, putting the corpse in the ambulance and taking it to the burial site - one pit for several bodies (ten and over). Another informant said there was no other option: washing the body and dressing for burial is preferred, but we have no choice, so [we] accept government’s recommendation. However, the group also requested to be trained for the work: Let the community be given the protective gear and advice so we can undertake the burial.
The normal burial process was then described, but rather briefly, with a stress on religious aspects: Previously [we] send a message to all families, then [a] meeting [is called] where the following is decided: [how to] provide food at home, [and] wash the body. Men wash men, women wash women. Moving the body around, for washing and for burying, is important information, because body-handling is bound to be a risky process in cases of Ebola death: bulky women are carried by men, [but] small[er] women can be carried by their women folk and back to the house (by hand). Then youths go and dig [the] grave, prayers are said over the dead, and the corpse is transported to the grave, which has been fitted in advance with an internal structure of board and sticks. The soil is then placed on the body after further prayers have been said.
When a wife dies, first it is required to report [the death] to [her] family and ask what should be done. The family grants permission to do the burial according to [her] religion. The husband is asked to bless, [and] forgive, and the imam offers general duwao [Arabic] asking for mercy. If the death was caused by sickness then sorcery [divination?] is done to find out the cause of the illness.
Female elders in Foindu provided specific information on procedures applied at the moment of death. First close the eyes of the dead person, [done] by the one who had being helping or taking care while she was sick. Also the mouth is closed. Both actions would pose an infection hazard in an Ebola case.
Then the body is moved from the bed, to prepare for washing, by two women, excluding those who have been helping, thus adding to the number of women at risk of cross-infection.
As many as six people take the dead for washing. Three wash her with white cloth, [satin] gloves, [and] hot water; if [she is] a Muslim zakat is given out from the cups of water, out of every ten cups of water one is left as zakat.
The corpse is then placed on a board and undressed by three women, who wash the corpse in a Muslim way by means of janaba. The washing of the corpse starts from the right hand from the head to the feet, then [turns to] the left side. Those washing the corpse first undertake the alwala.
The grave-digging is always done by men. They volunteer for the work to secure blessing. The workmen share tools: The same pickaxe and shovel are used by all. Further light is shed on the grave itself: Some graves have rooms where the corpse is placed and some do not.
In agreement with other groups, young people in Foindu objected to the way ‘safe burial’ was carried out. No, we don’t like it. [The] dead should be buried with honor and respect. Empower [the] community to bury our dead with full traditional rights; train us to perform the burial process.
Foindu youth offered much detail when it came to the burial process, as it used to be, before introduction of Ebola restrictions. When one is dead, female or male, family members will cry on the body, hold or touching the dead. After which the oldest of the family will inform the chief of the death. Chief then gives permission for the body to be prepared for burial.3
The potentially hazardous task of closing eyes and mouth is presented in a new light. People speak about severe sickness as being a time for the disclosure of hidden matters. Confession in such circumstances is thought to be advisable, even healthy. A woman with a difficult pregnancy may be told to confess the names of clandestine lovers. But the secrets of those close to death are handled with greater discretion. The eyes and mouth are closed by the wife or husband, or by the eldest child, because the person should be mature enough to keep the secrets of the dead.4
A summary of the burial process in Foindu compiled from comments by the three groups is set out in Appendix 2 (see page 155).
For a wider regional perspective on burial technique it is useful to compare information on Fogbo and Foindu with findings from a small village close to the Liberian border. Bo-Gaura is on the edge of the Gola forest reserve in Sembehun Section, Gaura chiefdom. It has no road, but is reached along a rutted, rock-strewn footpath. Techniques of the body deployed in undertaking in Bo-Gaura are essentially the same as those described for both Foindu and Fogbo, in the centre of the country.
The following account is compiled from remarks supplied by male elders:
The body is laid straight, eyes and mouth are closed and cloth spread over the body. The body is moved from the bed to the mat by four people. The place for washing the body is prepared at the back of the house. [This] is fenced with tarpaulin or mat and a hole dug where water will drain. Two pairs of gloves are given to the washing people. One scrubs the skin with soap and sapo [scrubbing material] and the other pours water. After washing the body, it is moved from the wet mat to a dry mat. The people who washed the body are responsible for dressing it. The person’s fine[est] dress is put on [the body] which is later wrapped in white satin and sprayed with perfume. Four young men are charged with the responsibility to take the corpse back home. The body is laid on a wooden coffin and taken to the house where it is officially handed over to the religious leader. Six youths take the body to the mosque and place it outside the mosque. Prayer is offered on the corpse and [it is] later taken to the grave.5
Sodality burial
Elders from Gbo chiefdom, in Bo District, offered some comments on sodality burial (see Appendix 3, page 156). The details are confidential and were not disclosed in the focus groups meetings. Sodality funerals are secret events - not ‘secret burials’ in the sense implied by Ebola responders, but closed events restricted only to members of the sodality.
Village-level concerns with ‘safe burial’
Teams of mainly younger people from urban areas were trained to carry out ‘safe burial’, equipped with transport, personal protective equipment (PPE) and chlorine sprays. With town-based vehicles in short supply, teams were at first slow to respond to calls for safe burial in more distant, inaccessible settlements such as Fogbo. It took burial teams four to five days to reach Bawuya to deal with the dead bodies of people infected by the Fogbo outbreak. In October 2014 Kenema District had only one burial team for the entire district, and it was heavily overstretched. Failure to reach suspected Ebola deaths after several days generally resulted in villagers burying the corpse as they saw fit.
Whether out of fear or pressure of work, burial teams appear, sometimes, to have used inappropriate methods:
The way they throw the corpses into the grave is the thing that I hate about the burial. These people cannot lay the corpse gently, but throw it. They don’t even wash the corpse, nor dress it respectfully.6
[The] dead are not handled with care and respect; male and female are [both] buried by male burial team; it is wrong: instead of holding the body, sticks are used to push dead bodies on to the stretcher.7
At times, rather than negotiate with uncooperative villagers, hard-pressed burial teams resorted to threats. In Peri Fefewabu (Gaura chiefdom) a rumour that chlorine spray was deadly appears to owe its origins to threats of this sort. They put fear into us and … were making threatening remarks. They said ‘we are spraying chlorine so that people will die’; The husband of the lady who first died of the disease [after attending a funeral in Liberia] survived and is still alive, but when they sprayed the chlorine, more people died.8
In other cases, burial teams carried out a dangerous job in difficult circumstances, and several villagers acknowledged it was a necessary task, and that team members were placing themselves at risk. The teams appear to have taken good care of their own safety. According to interviews in Bo with burial team personnel and management in December 2014 no cases of infection among the teams had been reported up to that time. Team members were, however, shunned by neighbours, and some were asked to leave their accommodation.
Villagers also took note that burial teams did not become infected, but this served to reinforce their conviction that they, too, could be trained to do the work.
We have seen [that] since the burial team [members] have been in this process none of them has been infected. We want the government to provide the protective gear used by the burial team so that we can bury the corpse without being infected.9
Disquiet at the work of burial teams was widely expressed across the sample. Since ‘safe burial’ applies to all deaths, whether of Ebola or not, then most if not all villages in Sierra Leone have by now experienced the work of the burial teams. The idea of villagers being trained and equipped to take over the work was raised without prompting in nearly a quarter of all focus group sessions. In settlements with Ebola cases this proportion rose to half.
The opinions expressed by focus groups in Baiima, Gbo chiefdom, and Foindu, summarized in Appendix 4 (see page 156), are typical of the larger data set.
A burial team perspective
Local responders - burial teams and contact tracers - came in for a lot of criticism from community members, but did a difficult and dangerous job with considerable commitment. Their viewpoint should also be represented.
A burial team manager10 reported that:
It is true there are areas we cannot get to easily because of bad terrain and no coverage for mobile phones. We were overstretched with few personnel in the burial teams, and very bad vehicles/burial vans. Command was scattered and [it was] difficult to locate who [needed us] and when. However [improvements are coming] with a command centre and coordinator. More vans have been provided. The workload has been divided. Now we have [agency name deleted] doing some burial, and areas of operation have been allotted, with more burial teams [deployed?] [Thus] the response is better these days compared to before. [But we need to] restrict movement to ease Ebola. With regards to cooperation and collaboration much improvement is [needed] ahead. On stigmatization: all I know [is that] my boys are stigmatized. Some say they are doing better this time. I also recommend that people change their perceptions of the burial teams, as [team members] are at risk. But none of them has [yet] been affected with Ebola. I recommend in the future to build [special] quarters to accommodate them.
A contact tracing officer11 commented on the muddle of mixed messaging that had derailed some of the response effort, and on evident problems with quarantine. He also connected the hazard posed by corpse-washing with the far from dignified nature of safe burial:
They said [Ebola] has no cure. This is why people [were] not going to the clinics/hospitals in the country. But now people are saying there is a cure. [This has] made the people to completely doubt the medical team [owing to mixed messages]. Let them use the [surviving] victims [to] talk to people; many are afraid. What is going wrong in the quarantined home is that food is not sufficient and some go around in the bush to seek for wood [firewood] and condiments. People can accept survivors if they possess discharge certificates and can be observed for another twenty-one days. The reason Ebola is still in the country is that people wash dead bodies before the arrival of the burial teams, and they [the teams] do not give dignified handling of the corpse as well as burial. It is true that members of the burial team are stigmatized as well as doctors and nurses. People are washing dead bodies, and [there is still] mass movement in and out of the villages and cities.
Undertaking
Calls to train community-based burial teams were loud and insistent. So why did this call fail to elicit a prompt response? Part of the problem was logistics. It was easier and quicker to mobilize and train teams at central locations, rather than in a distributed manner in communities. But part of the problem seems also to have been the way modern life ‘invents’ areas of ignorance concerning practical and necessary activities that have become thoroughly professionalized.12
WHO13 counselled empathy in regard to Ebola burial, but on what practical experience of burial was that empathy to be based?
As a child, on the backstreets of a Lancashire mill town, I lived opposite an undertaker’s premises, and thus had some familiarity with its daily routines - the power saw whining as boards for another coffin were cut to size, the comings and goings of the large black hearse, my grandfather standing to attention and taking off his hat when a newly filled coffin left the chapel of rest. I had no fear of (or ghoulish interest in) the corpses resting on the premises overnight; it was a family business, these were our neighbours, and to my five-year-old mind everything seemed perfectly normal.
But any such awareness of the daily routines of death has rapidly declined in developed countries. I would be hard pushed to know where I could now relive my childhood experiences. Since the nineteenth century body-handling at death has been professionalized, and then rationalized. In Britain, according to a fascinating study of the sociology of undertaking by Brian Parsons14 - the author himself by background an undertaker - the family undertaker largely disappeared at the end of the twentieth century owing to corporate rationalization.
Funeral directors’ premises may retain the external trappings of a family business offering a personalized service, but many are now part of large chains. The body may be taken to a local chapel of rest in the first instance, but is likely soon to be on its way in an unmarked refrigerated van around the urban ringway to a centralized cold store. Only once arrangements are in place for the funeral service, days or perhaps weeks later, will the body, now doubtless barcoded for track-and-trace monitoring, make its last and perhaps rather lengthy journey to a local place of cremation.
Parsons summarizes the story as follows:
A shift in ownership of funeral firms has occurred especially during the last three decades as independent organizations have been acquired by large organizations. This latter type of firm … exploited occupational control attributable to the rationalization of the death and disposal environment by managing their funeral operations on a centralized basis, thus achieving cost savings … a number of negative consequences are apparent … there is no evidence that [operational economies] are passed on to the consumer … retention of the original trading name deceives the public … [and] a degree of depersonalization exists.15
In short, undertaking has been industrialized, and escapes the everyday notice of the layperson in modern settings. Only the ritual of a funeral remains visible. It is perhaps not surprising that Ebola responders - many from backgrounds of the sort just described - tended to see funerals in Sierra Leone in terms only of ‘traditional ritual’, and missed the importance of training communities to transform body-handling technique, since this was part of the funeral process with which they had little or no direct experience.
As a result, procedures of body processing were misread as if they were rites, and judged strange, as if a proverbial visitor from Mars had stumbled across a broken-down white van full of frozen corpses in transit along a London ring road and had concluded the locals had a passion for necromantic joyriding.
Because local family-based body-processing techniques were also dangerous, by reason of Ebola risk, some responders concluded rather too quickly that West Africans were deliberately putting themselves, and the world, in danger through their stubborn persistence in performing traditional cultural rites.16
The problem was compounded by the seamless way in which local people, carrying out their own deeply felt responsibilities to the dead, wove together actions and meanings in their burial processes. The meanings arise from the actions, and are for this reason not easily separable. The grave cloth is muddied by the soil from the grave, and given as a keepsake to a child, who rushes in tears to the river to wash it, and the soil disappears down the stream as surely as the stream of the deceased person’s consciousness had ebbed away. The cloth, cleaned and dried, lives on as bedding for the child, and a tangible last link with a departed loved one. Action, materiality and signification are one.
Quarantine as technique
When an Ebola case is confirmed the patient is isolated, and high-risk contacts - basically people in the same household unit as the person with Ebola - are quarantined for twenty-one days. If there are subsequent cases, households are further quarantined, until the infection chain ends. The issue of how quarantine was applied, and by whom, and how it varied in urban and rural areas, is complex, and a fuller account requires further investigation. These comments, then, are provisional.
In Sierra Leone, quarantine was at times enforced by the security services (the army and police). Incidents of violence, of the kind experienced at West Point in Monrovia, seem to have been rather rare.17 In some cases, security personnel may have preferred not to grapple at close quarters with infected persons.
In a follow-up study undertaken in August 2015, in Peri Fefewabu, a village adjacent to the Gola forest, south of Kenema, where there were fourteen cases of Ebola in October 2104, we were told that close contacts of Ebola victims were quarantined in classrooms of the local primary school. Like many such premises, the primary school is on the outskirts of the settlement, separated from the dwelling area. The police and army maintained a cordon around the school, but sanctions on those attempting to break quarantine were imposed by local chiefs in the form of fines, and not by physical force.
In fact, the people of Peri praised the security services, since they had helped in bringing food, water and firewood to quarantined persons. The chiefs, we were told, used discretion in sanctioning quarantine breaches. Wanton breaches were fined, but not where delivery of emergency rations by Ebola responders was late or unforthcoming.
Some might say that this less draconian approach risked further spread of Ebola. Others might argue, however, that it helped establish that quarantine was a ‘commonsense’ measure. In effect, chiefly understanding of a basic human need for food might have facilitated a more general local acceptance of quarantine, honoured (in this case) in the breach. It is also worth adding that the Peri outbreak, like all other village outbreaks in the region, quickly came to an end. As will be shown in Chapter 6, local efforts in imposing quarantine and preventing unnecessary inter-village mobility had a significant impact on epidemic outcomes.
In part, these local efforts were successful because quarantine was not an alien idea to villagers. Enquiries uncovered numerous cases of public-spirited self-quarantine, undertaken to protect family, friends and neighbours. Focus group discussants pointed out that quarantine had been widely adopted by villagers to deal with disease threats such as smallpox in the past, and that the practice was still maintained to address ‘goat plague’ (PPR, peste des petits ruminants), a viral disease of sheep and goats in which infection occurs through contact with body fluids of infected animals, and which presents a useful model for thinking about Ebola.
Villagers are often aware (see focus group evidence collated in Appendix 5, page 157-8) that unless measures are undertaken to quarantine sick goats - sometimes by adopting strict community bye-laws - a village might easily lose all its goats. Furthermore, PPR, like Ebola, is an emergent disease in Sierra Leone, since it was introduced from other parts of Africa in the post-civil-war period, as a result of poorly managed animal restocking programmes.
Although by and large quarantine was rather readily accepted, this does not mean that villagers were satisfied with the way quarantine was managed. Some sensed, in particular, that responders made up the rules as they went along, and that they had not always thought through their protocols very thoroughly.
In Peri Fefewabu villagers were quick to comment on an inconsistency. Responders said there should be no home care, and that close family contacts should thus be isolated in the school, with each contact family group occupying one classroom. But nothing had been said about what should happen if one of the close contacts fell sick, other than to ring ‘117’ (in an area of little or no cell phone coverage!). Slow, or no, response by ‘117’ would in effect mean the household group was administering home care to an Ebola patient unaided, but now in a school classroom, without even the limited affordances that the home could provide. How was this reducing the infection risk, they wanted to know.
Villagers were also aware of, and confused by, some apparent bickering between different response agencies about the quarantine rules to be followed. There seemed to have been no agreed, general quarantine protocol among responders as late as October/November 2014.
There were also concerns about how close contacts, and indeed households, were defined. The frequently adopted ‘cooking pot’ definition of a household was probably the most relevant, in that the family feeding together probably organizes a lot of basic care of sick members together. Thereafter difficulty sets in, since ‘households’ (defined in this sense) do not map readily on to houses. Many buildings have two or more households within them. Some members of the same household may live apart, in separate buildings.
The international responders were directed in identifying people to be quarantined by their contact tracers, some of whom were perhaps too young and inexperienced for this kind of work. These contact tracers might be born in the village in question, and were available for work because schools had been closed. Typically they were at secondary school, perhaps in a nearby town. Their knowledge of precise, up-to-date sleeping arrangements might have been far from perfect. In some cases, finger-pointing may have owed more to local disputes than to Ebola exposure. Villagers in Peri Fefewabu implied that not all those exposed were quarantined, and not all those quarantined had been exposed.18
Again, the conclusion the villagers drew from this was that they should have been given the responsibility to design and implement their own quarantine rules, perhaps based on a revival of the old separation arrangements for smallpox victims. Every family has a farmhouse in the annual rice farm, and it is often an alternative place of residence for the nuclear family during the busy part of the farming season. It might have been better to organize isolation of Ebola patients in temporary shelters built near to farmhouses, as was the case with smallpox and other infectious diseases, than to use the local school. It would have been better to be quarantined close to a good source of food, water and fuel, to reduce the motive to break quarantine. The school was a choice reflecting the convenience, or lack of local knowledge, of external responders.
Actual quarantine breaches deserve closer study. They tend to be seen by responders as antisocial acts born of selfishness or ignorance. An Ebola infection chain in Sierra Leone in July/August 2015 stemmed from a quarantine breach by a man in his mid-twenties, living in Freetown. He ‘absconded’ at the end of Ramadan to be with his family in a village in Kholifah Rowalla chiefdom, Tonkolili District. In the daily bulletins of the National Ebola Response Commission, however, it is reported that he had a job in the city and was in the habit of returning to his village each month to bring his family food and money. He infected his uncle, who had taken charge of caring for the young man when he became sick. The mother’s brother is in effect a second father in the social conditions of rural Sierra Leone. An alleged moral ‘breach’, therefore, becomes on closer examination a picture of social responsibility and moral rectitude. The gap between social and medical norms is abundantly apparent.
Survivors
As of 23 August 2015, 28,041 people in Guinea, Liberia and Sierra Leone had been infected with Ebola, but 16,739 persons (59.7 per cent) had survived. Survival rates improved as rates of detection and availability of early palliative care improved. Survivors themselves contributed to this positive effect.
Survivors have two important embodied skills. They cannot be reinfected, so can safely touch and care for Ebola victims, and can be trained to do much of the work needed in Ebola care centres. Secondly, they provide tangible, living proof that the disease can be overcome. Ebola is not a death sentence. Accordingly, survivors have been used to spread positive messages about Ebola treatment, especially the message that early detection and admission greatly improve survival chances, as well as reducing risks to others.
However, survivors have suffered a degree of stigma, and some have been shunned by their communities. A particular problem is that the virus survives in semen, breast milk and the eyes for much longer than in blood or other body fluids. Survivors can convey the infection through sex or breastfeeding for many months after they have recovered from the disease. It is still not fully known how long this period lasts, or what risk of infection it poses. In particular, mixed messages about the period of sexual abstinence have proved confusing. Reintegration of survivors thus presents a range of unresolved challenges.
The following accounts provide a sense of what the disease does to its victims, and the problems they face. But these accounts also emphasize how survival is an opportunity to help others confront the disease.
I know Ebola is a dreadful disease because it has claimed the lives of my mother and [my] son (aged seven years). Ebola is caused by tombu [an entity which burrows inside the body] which cannot be seen with the eyes. We can contract [it] by contact with dead bodies, urine, faeces, sweat, blood, and through the eyes, cuts, and sperm from sexual intercourse. [In] my own case, [my sister and I] contracted it from my late mother who became ill a few days from return[ing] from a burial of one of our family members. She did not disclose how she contracted it until her death [probably this was revealed on the mother’s deathbed]. We were isolated when her result came in later, of Ebola. We were confused, stressed and isolated from the rest of our neighbours with whom we stay. We were quarantined with minimal food, [and with] police officers around with guns, which made us more depressed. Later, samples of blood [were taken], and the result was positive. I refused eating as the three of us were taken to the treatment centre at Bandajuma [MSF] camp. It was a miracle we were discharged and we are at home and feeling better, only that people in the neighbourhood do not visit us, even though we are all declared Ebola free … The food is not sufficient, and we have lost all our properties [clothes, bedding, furniture] because of Ebola - they were burnt. The good part is that we are free from any further outbreak for now, but the bad part is how can we recover our lost glory. I recommend that the government use all the victims on social interaction and health talk, to people who are in doubt [about] Ebola.19
I developed fever, with loss of appetite, vomiting and frequent stool. I thought of Ebola, because our mother died of it. At the treatment centre I summoned up courage and accepted conservative treatment. The good thing about the centre was that any food requested was provided. [After] a few days our brother died, which made us discouraged. I had sleepless nights, although I continued with the fluids, drinks, drugs taken, until miraculously I recovered. One day we were told Ebola has been conquered in our bodies, and we are to be discharged … The good thing of the treatment centre is that they encourage us - that is, the health personnel, and drugs and food were provided. [There were] counsellors around. Bad things [are that] we should have been provided with music and spiritual support. After discharge they should encourage the community we are living in for acceptance; [and] continue to educate the communities of affected victims to pay visits to them and not to isolate them. They should use us on social counselling of affected victims.20
Querying Ebola from the forest edge
The questionnaire interviews ended, according to our field team’s standard practice, by asking persons interviewed if they had questions of their own they would want the interviewer to write down and report. Many people availed themselves of the opportunity, and the questions they posed offer a fascinating insight into debates typical of what might be termed a village university of ‘people’s science’. Some of the confusions and contradictions of Ebola response are firmly nailed, with, at times, a quite delightful sense of irony and rhetoric.
The questions set out in Appendix 6 (see page 159) are especially worth pondering, since they reveal, for a set of communities with few if any roads and surrounded by the bats and monkeys presumed to be vectors of Ebola, some of the basic contradictions associated with the Upper West African epidemic.
Moreover, focus groups did not just discuss Ebola. They were also encouraged to talk about a range of other medical problems, to develop a sense of where Ebola sits in the larger picture of health concerns. Many groups commented on the neglect of other major diseases, notably malaria, owing to the national preoccupation with Ebola.
Men also often chose to talk about hernia. This is a major problem in farming communities heavily dependent on hand labour. A health system more oriented towards thinking in terms of techniques of the body, as Ebola now demands, might pay closer attention to hernia. The view of the male elders in Foindu was particularly explicit. It was, they said, a disease of ‘hard work’ and ‘poverty’. Treatment, ruinously expensive by village standards, was ‘by surgery, costing Le 1,500,000 at Makeni, plus vehicle charter - Le 200,000, or travel by transport vehicle - Le 50,000’. Deaths were reported. One man, without money for treatment, had suffered stomach pain for ten years, and was unable to walk. Deaths eventuated.
Convergence: thinking like an epidemiologist, and like a villager
Infection numbers began to level off, and then to fall, in the first affected districts of eastern Sierra Leone, from October 2014. A key factor was better survival rates. This depended on an important shift in medical perception - that the disease was more like cholera. Implementing best practice palliative care, to the highest standard, with a strong focus on rehydration, was said to be the key.21
It was at this point that some convergence became apparent between the thinking of international responders and affected communities. Simple messages configured around body technique underpinned home-care protocols - drink oral rehydration solution, or coconut water, nurse at a distance, only the patient handles the cup, one person only to be nominated as the caregiver, visitors and sympathizers to keep their distance.
Local skill and determination doubtless played a part in bringing about this shift. In evidence to be discussed in Chapter 6 one paramount chief trained and equipped his own locally based burial teams, and there was a rapid and significant reduction in further local spread of the disease.
Stories also began to emerge concerning attempts to improvise protective items from locally available materials such as plastic bags. One such improviser was a colleague, Roland Suluku, who made an Ebola ‘suit’ from cheap plastic sheeting. Commonsense application of basic knowledge concerning infection risks and rehydration requirements, plus determination, allowed some family members to pull through, where emergency calls for help went unanswered.
Such achievements, it transpired, were not unprecedented occurrences. Hewlett and Hewlett22 document how one woman in Gulu, northern Uganda, force-fed several members of her family on liquids and brought them through the 2000 epidemic. A young Liberian nursing student took a similar approach with three members of her own family, in this case attaching drips, and saving three of them. She protected herself through improvising protection with bin liners.23
Perhaps the most compelling evidence that villagers had begun to think like epidemiologists is to be found in the large appetite, evidenced above, for community-level training in safe burial. The message conveyed by these insistent demands is that the infection risks posed by burial had been accepted and understood. Help us now to beat the disease, was the gist of this local cry.
Bearing the risks of Ebola and the isolation of some forest-edge villages in mind, one female elder in Senehun Buima posed an exceptionally provocative question:
I’m a traditional birth attendant, we have pregnant women in our village. If it happens someone wants to put to bed [give birth] and we do not have medical equipment but local materials, how can we manage, because government says we should protect ourselves?
Clearly, the questioner implies, the authorities can stop burial, but they cannot stop birth. So the question conveys its own answer - more needs to be done to provide better in situ capacity to protect against Ebola infection. As will be shown in Chapter 6 this was not an impractical demand, even if more could and should have been done to support it.
But to travel down this path, even if only part of the way, implies international responders also made progress towards understanding the integration of village practices and social realities.
There is some evidence that a shift in this regard occurred as the epidemic in Sierra Leone approached its peak. By September 2014 WHO had included some home-care advice in its social mobilization prospectus, even while also stating plainly (and contradictorily) that such care was to be avoided. In November, six months into the epidemic in Sierra Leone, the Centers for Disease Control and Prevention (CDC) produced a poster entitled ‘Taking care of someone with suspected Ebola: be safe while you wait’.
Figure 5.1 ‘Taking care of someone with suspected Ebola: be safe while you wait’
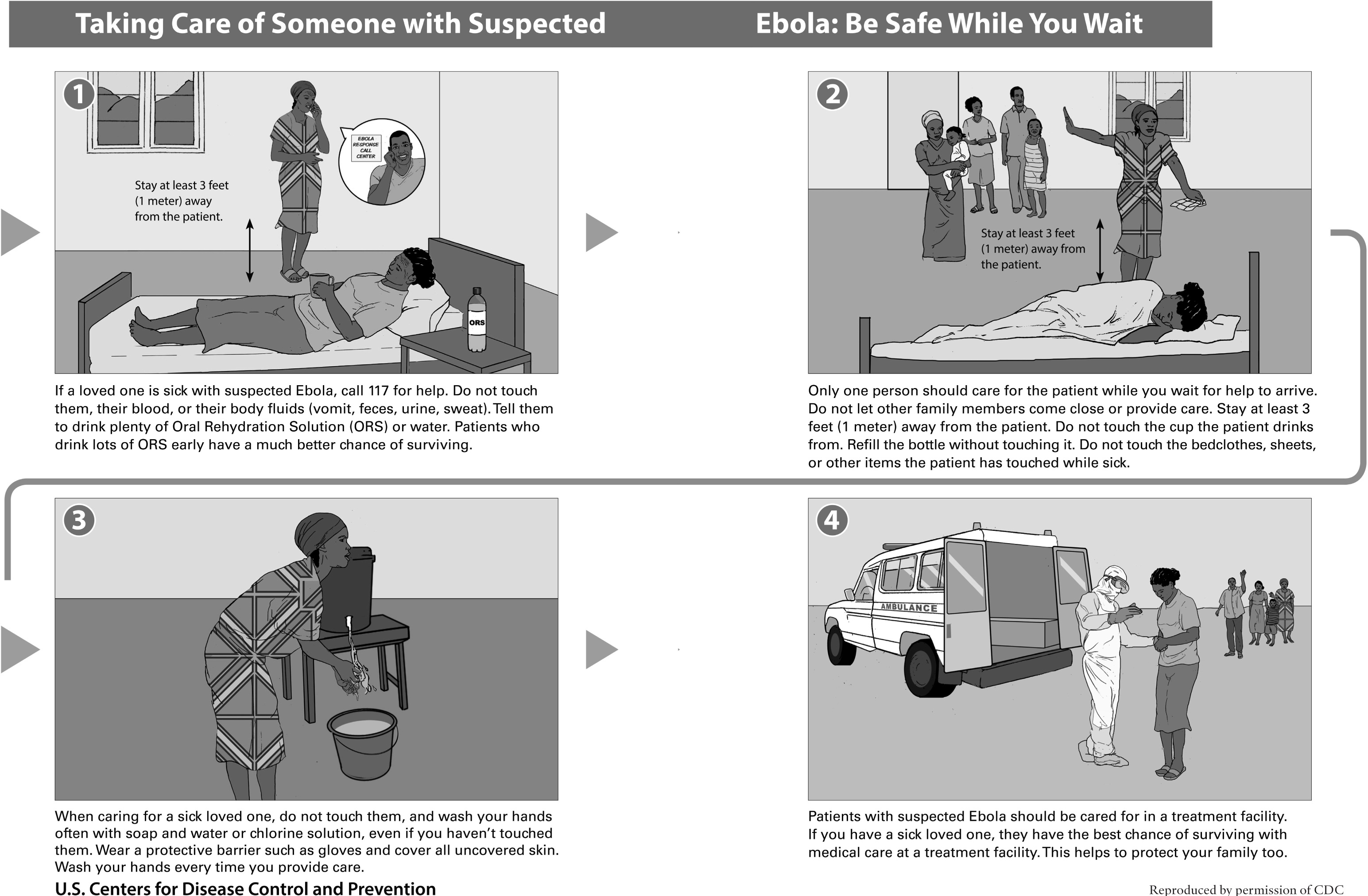
By entitling the poster ‘Be safe while you wait’ its designers cleverly avoided any clash between the medical mantra that there must be no home care and acceptance that some cases would receive help only after a long wait, or perhaps never. This, surely, is evidence that some epidemiologists were beginning to think like villagers, even if medical orthodoxy instructed them otherwise.
Equally, there is clear evidence of convergence from below. Foindu youths were either very attentive to the latest messages, or good at working things out for themselves, for they were aware of recommendations concerning one-on-one nursing and the use of bin liners even as that advice first began to circulate.
In mid-December 2014, only a matter of weeks after the CDC poster was issued, these young people summed up the process for the benefit of the Njala team:
The infected person is placed in a house by him/herself while other members are moved away. An elder of the family is appointed to provide care for this individual, through the use of black plastic bags to protect face, hands and feet from coming into contact with individual. This individual provides encouragement, support for the infected [person] until taken to the hospital. This elder may be very close family member (father, mother, child, sister or brother).24
Conclusion
Experience sooner or later persuaded local opinion that Ebola was a disease of body contact, and populations at risk began serious re-evaluation of techniques of the body associated with nursing the sick and burying the dead. Although passing on instructions was extensively adopted as a means of aligning local opinion with epidemiological viewpoints, in the expectation that information would drive behaviour, this chapter has presented some evidence that local ideas changed independently of the loudhailers. So much was happening at once, as the epidemic peaked, and the international surge kicked in, that it is hard to be certain about cause and effect. But there are several pieces of evidence to suggest some significant changes were driven from within. Perhaps one of the most secure facts, in this regard, is that provided by the young woman in Bo-Gaura, who remarked that a lurching hammock and a vomiting patient might be an infection risk for hammock carriers. I know of no messaging that mentioned hammocks as an infection risk, or that even acknowledged the existence of this most necessary item of village emergency medical kit, so this remark, surely, is an example of a villager understanding the implications of the disease within a context of local practices and social arrangements. There is evidence, also, that local people were proactive in reinforcing quarantine, in imposing movement restrictions, and in improvising protection to reduce risk of infection when handling Ebola cases. But above all there was a widely shared grassroots view that safe burial was something that communities could and should have been trained and equipped to undertake for themselves. This conviction ran quite against the grain of epidemic management thinking by external responders, in which the two words - ‘home care’ - were difficult to utter. So an issue arises, to be addressed in Chapter 6, about whether there was more scope for local agency than was at first assumed, and if so, how this aspect of Ebola response might have been better supported. In short, this final chapter will assess the hypothesis that local common sense helped end the epidemic.